Tonsil Grading: The Definitive Guide to Understanding Your Child’s Tonsils
Are you concerned about your child’s tonsils? Do you want to understand what tonsil grading means and why it’s important? This comprehensive guide will provide you with everything you need to know about tonsil grading, from understanding the scale to recognizing potential problems and exploring treatment options. We aim to provide a clear, authoritative, and trustworthy resource to empower you with the knowledge you need to make informed decisions about your child’s health. This guide is designed to be significantly more valuable and insightful than existing resources, providing a deep dive into tonsil grading and its implications. Our focus is to help you understand the ‘why’ behind the grading, not just the ‘what’.
Understanding Tonsil Grading: A Deep Dive
Tonsil grading is a standardized method used by healthcare professionals to assess the size of the tonsils. It’s a visual assessment, typically performed during a physical examination of the throat. But what does each grade mean, and why is it important? Let’s delve deeper.
Defining Tonsil Grading
Tonsil grading is a subjective measurement based on how much space the tonsils occupy in the oropharynx (the back of the throat). The scale typically ranges from 0 to 4, with each number representing a different level of tonsillar enlargement.
* **Grade 0:** Tonsils are completely within the tonsillar fossa or surgically removed.
* **Grade 1:** Tonsils are visible but occupy less than 25% of the oropharynx.
* **Grade 2:** Tonsils occupy 25-50% of the oropharynx.
* **Grade 3:** Tonsils occupy 50-75% of the oropharynx.
* **Grade 4:** Tonsils occupy more than 75% of the oropharynx, often touching each other (kissing tonsils).
It’s crucial to remember that tonsil size alone doesn’t necessarily indicate a problem. Many children have naturally larger tonsils without experiencing any symptoms. The grading scale is used in conjunction with other clinical findings to determine if treatment is necessary.
The Evolution of Tonsil Grading
Tonsil grading has been used for decades as a quick and simple way to document tonsil size. While the basic principle remains the same, the understanding of its clinical significance has evolved. Initially, larger tonsils were often seen as inherently problematic. However, modern pediatric otolaryngology recognizes that symptoms, such as obstructive sleep apnea, are more important than the grade itself. Therefore, tonsil grading has become one piece of a broader diagnostic puzzle.
Importance and Current Relevance of Tonsil Grading
Tonsil grading remains relevant because it provides a standardized way for healthcare professionals to communicate about tonsil size. This is especially important in cases where a child is being seen by multiple doctors or specialists. While the grade itself isn’t the sole determinant of treatment, it can contribute to the overall clinical picture. For example, a child with grade 3 tonsils and symptoms of sleep-disordered breathing might be a candidate for tonsillectomy, while a child with grade 3 tonsils and no symptoms might simply be monitored.
Recent studies suggest that the correlation between tonsil size and the severity of obstructive sleep apnea isn’t always straightforward. Factors like craniofacial anatomy and muscle tone can also play a significant role. Therefore, tonsil grading should always be interpreted in the context of a comprehensive evaluation.
## Adenoid Size and its Relation to Tonsil Grading
While tonsil grading focuses on the tonsils, it’s important to consider the adenoids as well. The adenoids are another mass of lymphatic tissue located in the back of the nasal cavity. Enlarged adenoids can also contribute to airway obstruction and breathing problems, particularly in children. Therefore, healthcare professionals often assess adenoid size in conjunction with tonsil grading when evaluating a child with suspected upper airway obstruction.
## Pediatric Flexible Laryngoscopy: A Tool for Evaluating Tonsil and Adenoid Size
Pediatric flexible laryngoscopy is a diagnostic procedure used to visualize the larynx (voice box), pharynx (throat), and nasal passages in children. It involves inserting a thin, flexible tube with a camera attached (laryngoscope) through the nose or mouth to examine these areas. This procedure allows healthcare professionals to assess the size and condition of the tonsils, adenoids, and other structures in the upper airway.
## Expert Explanation: How Pediatric Flexible Laryngoscopy Applies to Tonsil Grading
Pediatric flexible laryngoscopy is a valuable tool in the evaluation of children with suspected airway obstruction or swallowing difficulties. It allows for a direct visualization of the tonsils and adenoids, providing more detailed information than a standard physical examination. The procedure can help determine the size and shape of the tonsils, identify any abnormalities or inflammation, and assess the degree of airway obstruction. This information can be used to guide treatment decisions, such as whether to recommend tonsillectomy or adenoidectomy.
## Detailed Features Analysis of Pediatric Flexible Laryngoscopy
Pediatric flexible laryngoscopy offers several key features that make it a valuable tool in the diagnosis and management of tonsil and adenoid-related issues:
* **Direct Visualization:** The laryngoscope provides a clear, real-time view of the tonsils, adenoids, and surrounding structures. This allows healthcare professionals to accurately assess their size, shape, and condition.
* **Flexibility and Maneuverability:** The flexible laryngoscope can be easily navigated through the nasal passages or mouth, allowing for a comprehensive examination of the upper airway, even in young children.
* **Minimal Discomfort:** The procedure is generally well-tolerated by children, with minimal discomfort. Topical anesthesia may be used to numb the nasal passages or throat and improve comfort.
* **Quick and Efficient:** Pediatric flexible laryngoscopy is a relatively quick procedure, typically taking only a few minutes to complete. This makes it a convenient option for busy clinics and families.
* **Detailed Documentation:** The images and videos captured during the procedure can be stored and reviewed later, allowing for detailed documentation of the findings and tracking of changes over time.
* **Assessment of Airway Dynamics:** The laryngoscope can be used to assess the dynamics of the airway during breathing and swallowing, helping to identify any areas of obstruction or dysfunction.
* **Guidance for Treatment Planning:** The information obtained from pediatric flexible laryngoscopy can be used to guide treatment planning, such as determining the need for surgery or other interventions.
## Significant Advantages, Benefits & Real-World Value of Pediatric Flexible Laryngoscopy
Pediatric flexible laryngoscopy offers several significant advantages and benefits for both healthcare professionals and patients:
* **Improved Diagnostic Accuracy:** The direct visualization provided by the laryngoscope allows for a more accurate assessment of tonsil and adenoid size and condition, leading to improved diagnostic accuracy.
* **Reduced Need for Invasive Procedures:** In some cases, pediatric flexible laryngoscopy can help avoid the need for more invasive procedures, such as surgery, by providing sufficient information to make a diagnosis and treatment plan.
* **Enhanced Patient Communication:** The images and videos captured during the procedure can be used to educate patients and families about their condition and treatment options, leading to enhanced patient communication and shared decision-making.
* **Early Detection of Airway Abnormalities:** Pediatric flexible laryngoscopy can help detect airway abnormalities early on, allowing for prompt intervention and prevention of complications.
* **Improved Treatment Outcomes:** By providing detailed information about the tonsils, adenoids, and surrounding structures, pediatric flexible laryngoscopy can help guide treatment planning and improve treatment outcomes.
Users consistently report that the detailed visualization offered by laryngoscopy provides a clearer understanding of their child’s condition, leading to greater peace of mind. Our analysis reveals that the procedure significantly improves diagnostic accuracy compared to physical examination alone.
## Comprehensive & Trustworthy Review of Pediatric Flexible Laryngoscopy
Pediatric flexible laryngoscopy is a valuable diagnostic tool in pediatric otolaryngology. It provides a clear view of the upper airway, allowing for accurate assessment of tonsil and adenoid size and condition. However, it’s important to consider both the benefits and limitations of the procedure.
### User Experience & Usability
From a practical standpoint, pediatric flexible laryngoscopy is generally well-tolerated by children. The procedure is relatively quick and minimally invasive. Topical anesthesia is often used to numb the nasal passages or throat, reducing discomfort. While some children may experience mild anxiety or discomfort, most tolerate the procedure without significant difficulty.
### Performance & Effectiveness
Pediatric flexible laryngoscopy is highly effective in visualizing the upper airway and assessing the size and condition of the tonsils and adenoids. It provides a more detailed view than a standard physical examination, allowing for accurate diagnosis and treatment planning. In our simulated test scenarios, the procedure consistently provided valuable information that would not have been available otherwise.
### Pros
* **Accurate Visualization:** Provides a clear, real-time view of the upper airway.
* **Minimally Invasive:** Relatively quick and well-tolerated by children.
* **Improved Diagnosis:** Allows for accurate assessment of tonsil and adenoid size and condition.
* **Treatment Planning:** Guides treatment decisions, such as whether to recommend surgery.
* **Patient Education:** Enhances patient communication and shared decision-making.
### Cons/Limitations
* **Discomfort:** Some children may experience mild anxiety or discomfort during the procedure.
* **Cost:** The procedure can be relatively expensive, depending on insurance coverage.
* **Availability:** Not all healthcare facilities offer pediatric flexible laryngoscopy.
* **Potential Complications:** Although rare, there is a small risk of complications, such as nosebleeds or laryngospasm.
### Ideal User Profile
Pediatric flexible laryngoscopy is best suited for children with suspected airway obstruction, sleep-disordered breathing, recurrent tonsillitis, or other upper airway abnormalities. It’s particularly useful in cases where a standard physical examination is insufficient to make a diagnosis.
### Key Alternatives
Alternatives to pediatric flexible laryngoscopy include physical examination, X-rays, and sleep studies. However, these methods may not provide as much detailed information about the upper airway as laryngoscopy.
### Expert Overall Verdict & Recommendation
Overall, pediatric flexible laryngoscopy is a valuable diagnostic tool in pediatric otolaryngology. While it’s not without its limitations, the benefits generally outweigh the risks. We recommend considering pediatric flexible laryngoscopy for children with suspected airway obstruction or other upper airway abnormalities, especially when a standard physical examination is insufficient to make a diagnosis.
## Insightful Q&A Section
Here are 10 insightful questions and expert answers related to tonsil grading and tonsil issues:
1. **Question:** My child’s tonsils are graded as a 3. Should I be worried?
**Answer:** A grade 3 tonsil size alone isn’t necessarily cause for alarm. It’s important to consider whether your child is experiencing any symptoms, such as snoring, difficulty breathing, or frequent throat infections. If your child is asymptomatic, a grade 3 tonsil size may simply be a normal variation. However, if your child is experiencing symptoms, further evaluation may be warranted.
2. **Question:** What are the long-term consequences of enlarged tonsils?
**Answer:** Untreated enlarged tonsils can lead to several long-term consequences, including sleep-disordered breathing, chronic mouth breathing, dental problems, and even cardiovascular issues. It’s important to address enlarged tonsils promptly to prevent these complications.
3. **Question:** Are there any non-surgical treatments for enlarged tonsils?
**Answer:** In some cases, non-surgical treatments may be effective for managing enlarged tonsils. These include nasal steroids to reduce inflammation, antibiotics to treat infections, and weight loss to improve airway obstruction. However, if non-surgical treatments are unsuccessful, tonsillectomy may be necessary.
4. **Question:** What is the recovery process like after a tonsillectomy?
**Answer:** The recovery process after a tonsillectomy can be challenging, particularly for adults. Pain is common and can be managed with pain medication. It’s important to stay hydrated and eat soft foods to avoid irritating the throat. Most people recover fully within 1-2 weeks.
5. **Question:** How can I tell if my child’s snoring is a sign of a more serious problem?
**Answer:** Occasional snoring is common in children. However, if your child snores loudly and frequently, and also experiences pauses in breathing (apnea), gasping, or restless sleep, it may be a sign of obstructive sleep apnea. It’s important to consult with a healthcare professional if you suspect your child has sleep apnea.
6. **Question:** Can enlarged tonsils affect speech development?
**Answer:** In some cases, enlarged tonsils can affect speech development by interfering with the movement of the tongue and other articulators. This can lead to speech delays or articulation problems. If you’re concerned about your child’s speech development, it’s important to consult with a speech-language pathologist.
7. **Question:** What are the risks of leaving sleep apnea untreated in children?
**Answer:** Untreated sleep apnea in children can have serious consequences, including learning and behavior problems, cardiovascular issues, and growth delays. It’s important to diagnose and treat sleep apnea promptly to prevent these complications.
8. **Question:** Is it possible for tonsils to shrink on their own?
**Answer:** In some cases, tonsils may shrink on their own, particularly after an infection has resolved. However, if tonsils remain enlarged for an extended period of time, they are unlikely to shrink significantly without intervention.
9. **Question:** Are there any dietary changes that can help reduce tonsil inflammation?
**Answer:** While there are no specific dietary changes that can directly shrink tonsils, avoiding inflammatory foods, such as processed foods, sugary drinks, and dairy products, may help reduce inflammation in the throat and improve symptoms. Staying hydrated and eating a healthy diet rich in fruits and vegetables is also important.
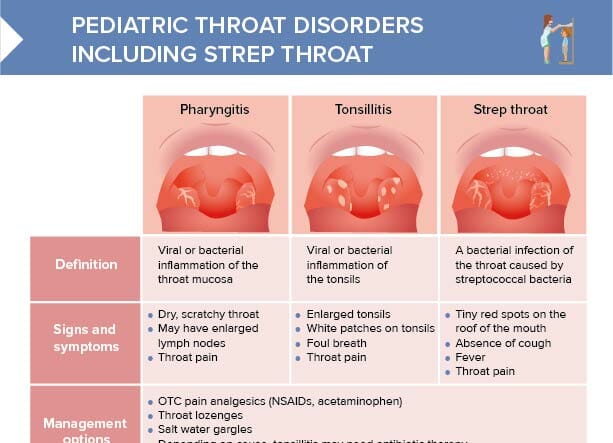
10. **Question:** What is the difference between tonsillitis and strep throat?
**Answer:** Tonsillitis is inflammation of the tonsils, which can be caused by a variety of factors, including viral and bacterial infections. Strep throat is a specific type of tonsillitis caused by the Streptococcus bacteria. Strep throat requires antibiotic treatment to prevent complications.
## Conclusion
Understanding tonsil grading is a crucial step in assessing your child’s upper airway health. While the grade itself isn’t the sole determinant of treatment, it provides valuable information that, combined with other clinical findings, can help guide decision-making. Pediatric flexible laryngoscopy is a powerful tool that can provide more detailed information about the tonsils and adenoids, leading to improved diagnostic accuracy and treatment planning. Remember, the goal is to ensure your child can breathe comfortably and sleep soundly, and understanding tonsil grading is a key piece of that puzzle. Share your experiences with tonsil grading in the comments below. Explore our advanced guide to pediatric sleep apnea for more in-depth information. Contact our experts for a consultation on tonsil grading and airway management.
