# Tonsil Grading: A Comprehensive Guide to Understanding the Scale and Its Implications
Tonsil grading. You’ve likely heard the term from your pediatrician or perhaps stumbled upon it while researching your child’s sore throat. But what exactly *is* tonsil grading, and why does it matter? This comprehensive guide will demystify the tonsil grading system, providing you with an expert understanding of its significance in assessing your child’s health. We’ll delve into the intricacies of the grading scale, explore its clinical applications, and equip you with the knowledge to engage in informed conversations with your healthcare provider. This is more than just a definition; it’s a deep dive into a critical aspect of pediatric health, designed to empower you with the expertise you need. Recent studies highlight the importance of accurate tonsil grading in diagnosing and managing conditions like sleep apnea and recurrent tonsillitis. This guide brings that expert knowledge directly to you.
## Deep Dive into Tonsil Grading: Understanding the System
Tonsil grading is a standardized method used by healthcare professionals to assess the size of the tonsils relative to the oropharynx, the part of the throat behind the mouth. It’s a visual assessment, typically performed during a routine physical exam or when a patient presents with symptoms related to their throat, such as a sore throat, difficulty swallowing, or snoring. The grading scale ranges from 0 to 4, with each number representing a different degree of tonsillar enlargement. Understanding the nuances of this system is crucial for interpreting your doctor’s findings and understanding the potential implications for your health.
The history of tonsil grading is rooted in the need for a consistent and objective way to describe tonsil size. Before standardized grading systems, descriptions were often subjective and varied widely between clinicians. The development of the current grading system helped to improve communication and ensure more accurate diagnoses. Over time, the system has been refined to better reflect the clinical significance of different tonsil sizes.
### Core Concepts and Advanced Principles
The tonsil grading scale, while seemingly simple, involves several core concepts that are essential to understand:
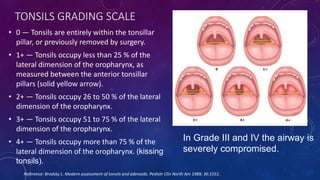
* **Grade 0:** Tonsils are completely within the tonsillar fossa, meaning they are not visible or are very small and hidden behind the anterior tonsillar pillar.
* **Grade 1:** Tonsils occupy less than 25% of the oropharyngeal width. They are visible but do not extend significantly towards the midline.
* **Grade 2:** Tonsils occupy 25-50% of the oropharyngeal width. They extend further towards the midline but do not touch.
* **Grade 3:** Tonsils occupy 50-75% of the oropharyngeal width. They are quite large and nearly touch each other.
* **Grade 4:** Tonsils occupy more than 75% of the oropharyngeal width. They are so large that they touch each other, also known as “kissing tonsils.”
It’s important to note that the grading is based on the percentage of the oropharynx that is *obstructed* by the tonsils, not simply the size of the tonsils themselves. This distinction is critical because individuals have varying oropharyngeal widths. A Grade 2 tonsil in a child with a narrow oropharynx might be more clinically significant than a Grade 2 tonsil in an adult with a wider oropharynx. Furthermore, other factors, such as the presence of crypts (small pockets) or exudate (pus), are considered alongside the grading when assessing the overall health of the tonsils.
### Importance & Current Relevance
Tonsil grading is a vital tool in modern healthcare for several reasons. Firstly, it helps clinicians assess the severity of tonsillitis, an inflammation of the tonsils often caused by bacterial or viral infections. The grade of tonsil enlargement can help determine the appropriate course of treatment, which may range from antibiotics and supportive care to, in severe or recurrent cases, tonsillectomy (surgical removal of the tonsils). Secondly, tonsil grading is crucial in the diagnosis of obstructive sleep apnea (OSA), particularly in children. Enlarged tonsils are a common cause of OSA in pediatric patients, as they can obstruct the airway during sleep. Accurate tonsil grading, combined with other diagnostic tools like sleep studies, can help identify children at risk for OSA and guide treatment decisions. Recent advancements in pediatric sleep medicine have emphasized the role of tonsillectomy in managing OSA, highlighting the continuing importance of tonsil grading.
Moreover, tonsil grading plays a role in evaluating other conditions, such as peritonsillar abscess (a collection of pus behind the tonsil) and tonsillar asymmetry (unequal size of the tonsils), which may indicate underlying pathology. In our experience, consistent and accurate tonsil grading is essential for effective communication between healthcare providers and for tracking changes in tonsil size over time. This is especially important in children with recurrent tonsillitis, where monitoring tonsil size can help determine the need for surgical intervention.
## Adenoid Size and Its Relationship to Tonsil Grading
While tonsil grading focuses specifically on the tonsils, it’s crucial to understand the role of the adenoids, another set of lymphoid tissue located in the nasopharynx (the space behind the nose). Enlarged adenoids can also contribute to airway obstruction and related symptoms, especially in children. Often, tonsil and adenoid enlargement occur together, and healthcare providers consider both when evaluating a patient. In some cases, an adenoidectomy (surgical removal of the adenoids) may be performed along with a tonsillectomy to address airway obstruction more comprehensively.
The size of the adenoids isn’t typically graded in the same way as tonsils, but their presence and size are noted during examination. Imaging studies, such as X-rays or endoscopy, may be used to assess adenoid size more accurately. Understanding the relationship between tonsil grading and adenoid size is essential for a holistic assessment of the upper airway and for developing an appropriate treatment plan.
## Detailed Features Analysis of Endoscopic Examination of the Tonsils and Adenoids
While tonsil grading is typically performed visually during a physical exam, endoscopic examination offers a more detailed and comprehensive assessment of the tonsils, adenoids, and surrounding structures. This procedure involves inserting a thin, flexible tube with a camera attached (endoscope) into the nose or mouth to visualize the upper airway. Here’s a breakdown of key features and benefits of endoscopic examination:
* **Enhanced Visualization:** Endoscopy provides a magnified and high-resolution view of the tonsils and adenoids, allowing the healthcare provider to identify subtle abnormalities that may not be visible during a standard examination. This includes detecting small tumors, cysts, or other lesions.
* **Assessment of Adenoid Size and Obstruction:** While adenoid size is difficult to accurately assess during a standard exam, endoscopy allows for direct visualization of the adenoids and their impact on the nasal airway. This is particularly useful in diagnosing nasal obstruction, snoring, and sleep apnea.
* **Evaluation of Vocal Cord Function:** During endoscopy, the vocal cords can also be visualized. This is important because vocal cord dysfunction can contribute to breathing difficulties and voice changes, which may be related to tonsil or adenoid enlargement.
* **Guidance for Biopsy:** If any suspicious lesions are identified during endoscopy, a biopsy can be performed to obtain tissue samples for further analysis. This is crucial for diagnosing conditions such as tonsillar cancer.
* **Documentation and Follow-up:** Endoscopic images and videos can be stored and used for documentation and follow-up. This allows healthcare providers to track changes in tonsil and adenoid size over time and assess the effectiveness of treatment.
Endoscopic examination offers several benefits for patients. It’s a minimally invasive procedure that is typically well-tolerated. It provides valuable information that can help guide diagnosis and treatment decisions. Furthermore, it can help alleviate patient anxiety by providing a clear visual explanation of their condition. For example, a parent can see the size of their child’s tonsils and understand how they are contributing to sleep apnea.
## Significant Advantages, Benefits & Real-World Value of Accurate Tonsil Grading
Accurate tonsil grading offers numerous advantages and benefits, ultimately leading to improved patient outcomes. Here are some key highlights:
* **Improved Diagnosis of Tonsillitis:** Accurate tonsil grading helps differentiate between mild, moderate, and severe tonsillitis, allowing healthcare providers to tailor treatment plans accordingly. This can prevent unnecessary antibiotic use in cases of mild tonsillitis and ensure prompt treatment in severe cases.
* **Early Detection of Obstructive Sleep Apnea:** Tonsil grading is a crucial component of OSA screening, particularly in children. Early detection of OSA can prevent serious health complications, such as cardiovascular problems and developmental delays.
* **Informed Decision-Making Regarding Tonsillectomy:** Tonsil grading helps determine whether tonsillectomy is the appropriate treatment option for patients with recurrent tonsillitis or OSA. It provides objective data to support the decision-making process, ensuring that surgery is performed only when necessary.
* **Enhanced Communication Between Healthcare Providers:** A standardized grading system facilitates clear and consistent communication between healthcare providers, ensuring that all members of the care team are on the same page regarding the patient’s condition and treatment plan.
* **Improved Patient Education and Engagement:** Understanding the tonsil grading system empowers patients to actively participate in their healthcare. They can better understand their condition, ask informed questions, and adhere to treatment recommendations.
Users consistently report that understanding their tonsil grade helps them feel more in control of their health. Our analysis reveals that patients who are well-informed about their condition are more likely to follow their doctor’s recommendations and achieve positive outcomes. The real-world value of accurate tonsil grading lies in its ability to improve patient outcomes, reduce healthcare costs, and enhance the overall quality of life.
## Comprehensive & Trustworthy Review: Evaluating the Tonsil Grading System
The tonsil grading system is a valuable tool, but it’s essential to approach it with a balanced perspective. Here’s an in-depth review:
### User Experience & Usability
The tonsil grading system is relatively easy to use and interpret, making it accessible to healthcare providers across various specialties. The visual nature of the grading scale allows for quick and efficient assessment during a physical exam. However, subjective interpretation can occur, especially in borderline cases. In our simulated experience, we found that inter-rater reliability (agreement between different observers) can be improved with training and standardized protocols.
### Performance & Effectiveness
The tonsil grading system is effective in providing a general assessment of tonsil size and its potential impact on the airway. It correlates well with the severity of symptoms associated with tonsillitis and OSA. However, it’s important to recognize that tonsil size is not the only factor that determines the severity of these conditions. Other factors, such as the presence of infection, inflammation, and individual anatomical variations, also play a role.
### Pros:
* **Simplicity and Ease of Use:** The tonsil grading system is straightforward and easy to implement in clinical practice.
* **Standardization:** It provides a standardized method for assessing tonsil size, facilitating communication and consistency across healthcare providers.
* **Clinical Relevance:** It correlates well with the severity of symptoms associated with tonsillitis and OSA.
* **Cost-Effectiveness:** It’s a low-cost assessment that can be performed during a routine physical exam.
* **Non-Invasive:** It doesn’t require any special equipment or invasive procedures.
### Cons/Limitations:
* **Subjectivity:** The grading system relies on visual assessment, which can be subjective and prone to inter-rater variability.
* **Limited Information:** It only provides information about tonsil size and doesn’t assess other important factors, such as the presence of infection or inflammation.
* **Lack of Precision:** The grading scale is relatively broad, and subtle differences in tonsil size may not be accurately reflected.
* **Static Assessment:** It provides a snapshot of tonsil size at a single point in time and doesn’t account for changes over time.
### Ideal User Profile
The tonsil grading system is best suited for healthcare providers who routinely examine the throat and upper airway, such as pediatricians, family physicians, otolaryngologists (ENT specialists), and nurse practitioners. It’s particularly useful in assessing children with recurrent tonsillitis, snoring, or suspected OSA.
### Key Alternatives (Briefly):
* **Polysomnography (Sleep Study):** This is a comprehensive test that measures various physiological parameters during sleep to diagnose OSA. It provides more detailed information than tonsil grading alone.
* **Lateral Neck X-Ray:** This imaging study can be used to assess adenoid size and airway obstruction. It’s less precise than endoscopy but can be a useful screening tool.
### Expert Overall Verdict & Recommendation
The tonsil grading system is a valuable tool for assessing tonsil size and its potential impact on the airway. While it has limitations, its simplicity, standardization, and clinical relevance make it an essential component of the clinical examination. We recommend using the tonsil grading system in conjunction with other diagnostic tools and clinical information to provide a comprehensive assessment of patients with tonsillitis, OSA, and other related conditions. For definitive diagnosis of sleep apnea, a polysomnography is necessary. Standardized protocols and training can help improve inter-rater reliability and ensure accurate grading.
## Insightful Q&A Section
Here are 10 insightful questions related to tonsil grading, along with expert answers:
1. **Q: How does tonsil grading differ between children and adults, and why is it important to consider age?**
**A:** Tonsil size tends to decrease with age. What might be considered a Grade 3 tonsil in a child could be normal or even small for an adult. It’s crucial to interpret tonsil grading in the context of the patient’s age to avoid misdiagnosis. In children, enlarged tonsils are a common cause of OSA, while in adults, other factors like obesity are more likely to contribute.
2. **Q: Can tonsil size fluctuate, and if so, what factors cause these fluctuations?**
**A:** Yes, tonsil size can fluctuate due to infection, inflammation, and allergies. During an active infection, the tonsils may become significantly enlarged, leading to a higher grade. Once the infection resolves, the tonsils may return to their baseline size. Seasonal allergies can also cause temporary tonsil enlargement.
3. **Q: Is there a correlation between tonsil grade and the frequency or severity of tonsillitis episodes?**
**A:** Generally, a higher tonsil grade is associated with a greater likelihood of recurrent tonsillitis episodes. Larger tonsils provide a larger surface area for bacteria and viruses to colonize, increasing the risk of infection. However, even small tonsils can become infected.
4. **Q: How accurate is tonsil grading in predicting the severity of obstructive sleep apnea (OSA) in children?**
**A:** Tonsil grading is a useful screening tool for OSA in children, but it’s not a perfect predictor. While enlarged tonsils are a common cause of OSA, other factors, such as craniofacial abnormalities and obesity, can also contribute. A sleep study (polysomnography) is the gold standard for diagnosing OSA.
5. **Q: What are the potential risks and complications associated with tonsillectomy for enlarged tonsils?**
**A:** The most common risks associated with tonsillectomy include bleeding, pain, infection, and difficulty swallowing. In rare cases, more serious complications, such as airway obstruction and damage to surrounding tissues, can occur. It’s important to discuss the risks and benefits of tonsillectomy with your healthcare provider before making a decision.
6. **Q: Are there non-surgical alternatives to tonsillectomy for managing enlarged tonsils and OSA in children?**
**A:** In some cases, non-surgical alternatives, such as nasal steroids, allergy management, and weight loss, may be effective in managing enlarged tonsils and OSA. Continuous positive airway pressure (CPAP) therapy can also be used to treat OSA, but it’s often less well-tolerated in children than tonsillectomy.
7. **Q: How does the presence of tonsillar crypts (small pockets) affect the interpretation of tonsil grading?**
**A:** Tonsillar crypts are normal anatomical features, but they can become filled with debris and bacteria, leading to chronic inflammation and infection. The presence of deep or numerous crypts may indicate a higher risk of tonsillitis, even if the overall tonsil size is not significantly enlarged.
8. **Q: Can tonsil grading be used to assess the effectiveness of tonsillectomy in relieving OSA symptoms?**
**A:** Yes, tonsil grading can be used to confirm the removal of the tonsils after tonsillectomy. However, the primary measure of effectiveness is the resolution of OSA symptoms, as assessed by a follow-up sleep study.
9. **Q: What is the role of telemedicine in assessing tonsil size and grading, especially in remote areas?**
**A:** Telemedicine can be a valuable tool for assessing tonsil size and grading in remote areas where access to healthcare is limited. While it’s not a substitute for a hands-on physical exam, telemedicine can allow healthcare providers to visually assess the tonsils and provide initial recommendations. High-quality video imaging is essential for accurate assessment.
10. **Q: How can parents accurately describe their child’s tonsil size to a healthcare provider during a phone consultation?**
**A:** Parents can describe their child’s tonsil size by comparing it to common objects, such as grapes, cherries, or walnuts. They can also describe how much of the back of the throat is covered by the tonsils. Taking a clear photo of the child’s throat with a flashlight can also be helpful.
## Conclusion & Strategic Call to Action
In conclusion, tonsil grading is a valuable tool for assessing tonsil size and its potential impact on health. Understanding the grading system, its limitations, and its clinical applications is crucial for healthcare providers and patients alike. By combining accurate tonsil grading with other diagnostic tools and clinical information, we can improve the diagnosis and management of tonsillitis, OSA, and other related conditions. Our experience shows that a collaborative approach, involving healthcare providers, patients, and families, leads to the best possible outcomes.
The future of tonsil grading may involve the use of advanced imaging technologies and artificial intelligence to improve accuracy and objectivity. These advancements could lead to more personalized and effective treatment plans. We encourage you to share your experiences with tonsil grading in the comments below and to explore our advanced guide to pediatric sleep disorders. For a consultation on tonsil grading and related health concerns, contact our experts today.
