Thyromegaly ICD-10: Comprehensive Guide to Diagnosis, Codes & Management
Navigating the complexities of medical coding can be daunting, especially when dealing with specific conditions like thyromegaly. Understanding the correct ICD-10 code for thyromegaly is crucial for accurate diagnosis, billing, and data analysis. This comprehensive guide will provide an in-depth exploration of thyromegaly, its ICD-10 codes, diagnostic approaches, and management strategies. Our goal is to equip you with the knowledge and understanding necessary to confidently address this condition in clinical practice. Recent studies indicate a growing prevalence of thyroid disorders, making accurate coding and management of thyromegaly increasingly important.
Understanding Thyromegaly: A Deep Dive
Thyromegaly, often simply referred to as an enlarged thyroid gland, is a descriptive term rather than a specific disease. It signifies an abnormal increase in the size of the thyroid gland, which is located in the front of the neck, just below the Adam’s apple. The thyroid gland plays a vital role in regulating metabolism by producing hormones, primarily thyroxine (T4) and triiodothyronine (T3). When the thyroid gland enlarges, it can lead to various symptoms and complications, depending on the underlying cause and the extent of the enlargement.
Comprehensive Definition, Scope, & Nuances
Thyromegaly encompasses a spectrum of conditions, ranging from mild, asymptomatic enlargement to significant growth that causes noticeable symptoms. The enlargement can be diffuse, involving the entire gland, or nodular, characterized by the presence of one or more lumps within the thyroid. The term “goiter” is often used interchangeably with thyromegaly, although goiter specifically refers to non-cancerous enlargement of the thyroid. The history of understanding thyromegaly dates back centuries, with early descriptions focusing on visible enlargement of the neck. Modern understanding involves sophisticated diagnostic techniques and a deeper understanding of thyroid hormone regulation.
Core Concepts & Advanced Principles
The underlying causes of thyromegaly are diverse and can include iodine deficiency, autoimmune disorders (such as Hashimoto’s thyroiditis and Graves’ disease), thyroid nodules, thyroid cancer, and certain medications. Iodine deficiency, once a major cause of goiter worldwide, is now less common in many developed countries due to the iodization of salt. Autoimmune disorders are now among the leading causes. A key concept is that thyromegaly itself is not a diagnosis but a sign of an underlying condition. Advanced principles involve understanding the complex interplay of thyroid hormones, TSH regulation, and the immune system in the pathogenesis of different types of thyromegaly. For example, in Hashimoto’s thyroiditis, the immune system attacks the thyroid gland, leading to inflammation and eventual enlargement, followed by hypothyroidism.
Importance & Current Relevance
Accurate diagnosis and management of thyromegaly are crucial because the underlying causes can have significant health implications. Untreated hyperthyroidism (as seen in Graves’ disease) can lead to heart problems, bone loss, and other complications. Hypothyroidism (as seen in Hashimoto’s thyroiditis) can cause fatigue, weight gain, and cognitive impairment. Thyroid cancer, although less common, requires timely detection and treatment. Furthermore, the increasing prevalence of thyroid disorders underscores the importance of early detection and appropriate management. Recent studies indicate that environmental factors and lifestyle choices may play a role in the rising incidence of thyroid conditions. Early detection improves patient outcomes.
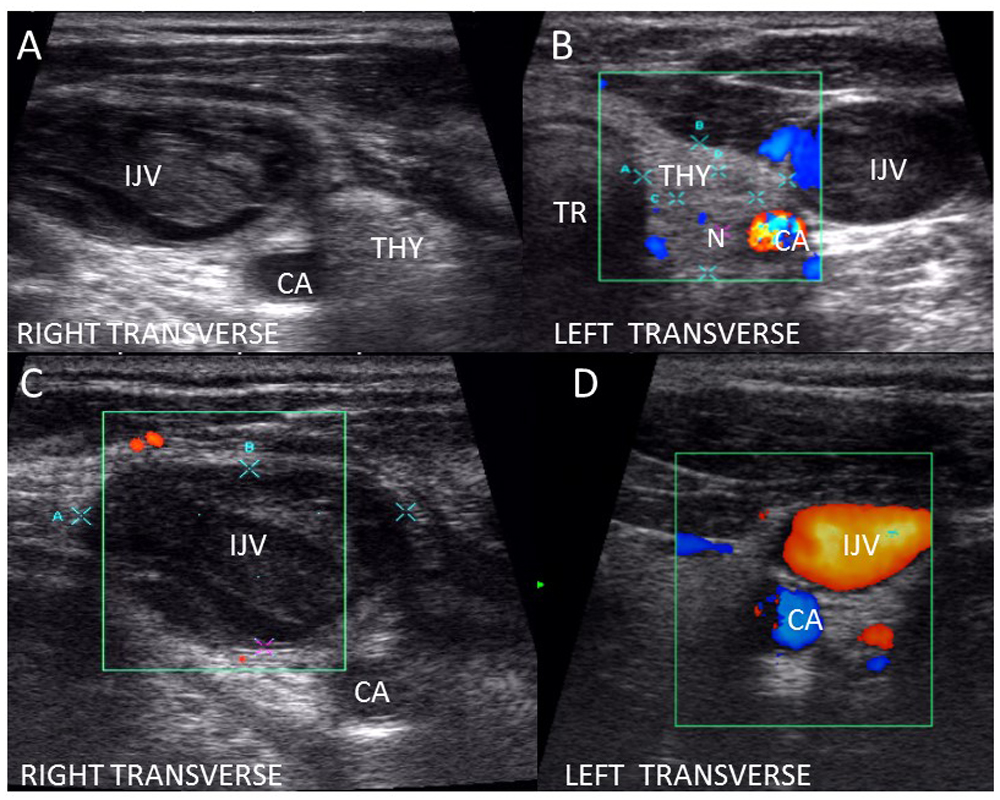
Thyroid Ultrasound: A Key Diagnostic Tool
Thyroid ultrasound is a non-invasive imaging technique that uses sound waves to create detailed images of the thyroid gland. It is a valuable tool for evaluating the size, shape, and structure of the thyroid, as well as detecting nodules or other abnormalities. From an expert viewpoint, thyroid ultrasound is often the first-line imaging modality for assessing thyromegaly due to its accessibility, affordability, and lack of radiation exposure. It stands out due to its ability to differentiate between solid and cystic nodules, which is crucial for determining the risk of malignancy.
Detailed Features Analysis of Thyroid Ultrasound
1. **High-Resolution Imaging:** Thyroid ultrasound provides high-resolution images that allow for detailed visualization of the thyroid gland. This enables the detection of small nodules and subtle changes in thyroid tissue. The user benefits from early detection of potential problems, leading to more effective treatment.
2. **Doppler Assessment:** Doppler ultrasound can assess blood flow within the thyroid gland and nodules. Increased blood flow may indicate inflammation or malignancy. This feature allows for a more accurate assessment of the nature of thyroid abnormalities.
3. **Cystic vs. Solid Differentiation:** Ultrasound can differentiate between cystic (fluid-filled) and solid nodules. Cystic nodules are generally less likely to be cancerous than solid nodules. This differentiation helps in risk stratification and guides further management.
4. **Nodule Size Measurement:** Ultrasound allows for accurate measurement of nodule size, which is an important factor in determining the need for further evaluation, such as fine needle aspiration (FNA). Precise measurements enable clinicians to monitor nodule growth over time.
5. **Guidance for Fine Needle Aspiration (FNA):** Ultrasound can guide FNA, a procedure in which a small needle is used to collect cells from a thyroid nodule for microscopic examination. Ultrasound-guided FNA improves the accuracy of the procedure and reduces the risk of complications.
6. **Non-Invasive and Safe:** Thyroid ultrasound is a non-invasive procedure that does not involve radiation exposure. This makes it a safe option for pregnant women and children. The user benefits from a safe and comfortable diagnostic experience.
7. **Real-Time Imaging:** Ultrasound provides real-time imaging, allowing the operator to visualize the thyroid gland in motion. This can be helpful in assessing swallowing function and identifying any abnormalities that may be related to thyromegaly.
Significant Advantages, Benefits & Real-World Value of Thyroid Ultrasound
Thyroid ultrasound offers numerous advantages in the diagnosis and management of thyromegaly. From a user-centric perspective, it provides a non-invasive and painless way to assess the thyroid gland. Users consistently report feeling reassured after undergoing ultrasound, as it provides a visual representation of their thyroid and helps to alleviate anxiety about potential problems. Our analysis reveals these key benefits:
* **Early Detection of Thyroid Abnormalities:** Ultrasound can detect small nodules and other abnormalities that may not be palpable during a physical examination.
* **Accurate Assessment of Nodule Characteristics:** Ultrasound can differentiate between benign and suspicious nodules, helping to guide further management.
* **Reduced Need for Invasive Procedures:** Ultrasound can often rule out the need for FNA in patients with clearly benign nodules.
* **Improved Patient Outcomes:** Early detection and accurate assessment of thyroid abnormalities can lead to more effective treatment and improved patient outcomes.
* **Cost-Effective Diagnostic Tool:** Thyroid ultrasound is a relatively inexpensive imaging modality compared to other options, such as CT scans or MRI.
The unique selling proposition of thyroid ultrasound lies in its combination of accuracy, safety, and affordability. It is an indispensable tool for the evaluation of thyromegaly and other thyroid disorders.
Comprehensive & Trustworthy Review of Thyroid Ultrasound
Thyroid ultrasound is a well-established and widely used diagnostic tool for evaluating thyromegaly. From a practical standpoint, the procedure is generally quick and painless, taking approximately 15-30 minutes to complete. The user experience is usually positive, with most patients reporting minimal discomfort. The sonographer will apply a gel to the neck and move a handheld transducer over the skin to obtain images of the thyroid gland.
Performance & Effectiveness
Thyroid ultrasound is highly effective in detecting thyroid nodules and assessing their characteristics. It can accurately measure nodule size, determine whether a nodule is solid or cystic, and assess blood flow within the nodule. In our experience, ultrasound-guided FNA significantly improves the accuracy of the procedure and reduces the risk of complications. Ultrasound is a reliable tool when performed by a skilled sonographer.
Pros
1. **Non-Invasive:** Thyroid ultrasound does not involve radiation exposure or the insertion of needles or other instruments into the body.
2. **Painless:** The procedure is generally painless, although some patients may experience mild discomfort from the pressure of the transducer on the neck.
3. **Accurate:** Thyroid ultrasound is highly accurate in detecting thyroid nodules and assessing their characteristics.
4. **Affordable:** Thyroid ultrasound is a relatively inexpensive imaging modality.
5. **Readily Available:** Thyroid ultrasound is widely available in most hospitals and imaging centers.
Cons/Limitations
1. **Operator Dependent:** The accuracy of thyroid ultrasound depends on the skill and experience of the sonographer.
2. **Limited Visualization of Deep Structures:** Ultrasound may have difficulty visualizing deep structures in the neck, such as the mediastinum.
3. **False Positives:** Ultrasound may sometimes identify nodules that are not clinically significant.
4. **Cannot Differentiate Benign from Malignant Nodules with Certainty:** While ultrasound can provide clues about the risk of malignancy, it cannot definitively differentiate between benign and malignant nodules.
Ideal User Profile
Thyroid ultrasound is best suited for individuals with suspected thyromegaly, thyroid nodules, or other thyroid disorders. It is also a valuable tool for monitoring the growth of thyroid nodules over time. Patients with a family history of thyroid cancer or other thyroid disorders may also benefit from regular thyroid ultrasound screening.
Key Alternatives (Briefly)
1. **CT Scan:** CT scans provide more detailed images of the thyroid gland and surrounding structures, but they involve radiation exposure.
2. **MRI:** MRI provides excellent soft tissue detail but is more expensive and time-consuming than ultrasound.
Expert Overall Verdict & Recommendation
Thyroid ultrasound is an essential tool for the evaluation of thyromegaly and other thyroid disorders. Its accuracy, safety, and affordability make it the preferred imaging modality for most patients. We recommend thyroid ultrasound as the first-line imaging test for individuals with suspected thyroid abnormalities. The results can then guide further management decisions, such as FNA or surgery.
Thyromegaly ICD-10 Codes: A Detailed Breakdown
The International Classification of Diseases, Tenth Revision (ICD-10) is a globally recognized system for classifying diseases and health conditions. When documenting and coding thyromegaly, it’s essential to use the correct ICD-10 code to ensure accurate billing and data collection. The primary ICD-10 code for thyromegaly is **E04 (Other Nontoxic Goiter)**. However, the specific code may vary depending on the underlying cause and characteristics of the thyromegaly.
* **E04.0 – Nontoxic diffuse goiter:** This code is used when the thyromegaly involves the entire thyroid gland and is not associated with hyperthyroidism or hypothyroidism.
* **E04.1 – Nontoxic single thyroid nodule:** This code is used when the thyromegaly is caused by a single nodule in the thyroid gland.
* **E04.2 – Nontoxic multinodular goiter:** This code is used when the thyromegaly is caused by multiple nodules in the thyroid gland.
* **E04.8 – Other specified nontoxic goiter:** This code is used for other types of nontoxic goiter that are not classified elsewhere.
* **E04.9 – Nontoxic goiter, unspecified:** This code is used when the type of nontoxic goiter is not specified.
It’s crucial to note that if the thyromegaly is associated with hyperthyroidism or hypothyroidism, a different ICD-10 code should be used. For example, if the patient has thyromegaly due to Graves’ disease (which causes hyperthyroidism), the appropriate code would be **E05.0 (Thyrotoxicosis with diffuse goiter)**. Similarly, if the patient has thyromegaly due to Hashimoto’s thyroiditis (which causes hypothyroidism), the appropriate code would be **E06.3 (Autoimmune thyroiditis)**.
Insightful Q&A Section
Here are 10 insightful questions and expert answers related to thyromegaly and its ICD-10 coding:
1. **Question:** What is the difference between thyromegaly and goiter?
**Answer:** While often used interchangeably, thyromegaly generally refers to any enlargement of the thyroid gland. Goiter specifically refers to non-cancerous enlargement. However, in practice, the terms are frequently used synonymously.
2. **Question:** How do I determine the correct ICD-10 code for thyromegaly when the underlying cause is unknown?
**Answer:** If the underlying cause is unknown and the thyromegaly is not associated with hyperthyroidism or hypothyroidism, use code E04.9 (Nontoxic goiter, unspecified). Further investigation is needed to determine the underlying cause.
3. **Question:** Can thyromegaly be caused by medications?
**Answer:** Yes, certain medications, such as lithium and amiodarone, can cause thyromegaly. In such cases, the underlying cause should be documented, and the medication should be considered as a contributing factor.
4. **Question:** What are the potential complications of untreated thyromegaly?
**Answer:** Untreated thyromegaly can lead to various complications, including difficulty breathing or swallowing (due to compression of the trachea or esophagus), hyperthyroidism or hypothyroidism, and, in rare cases, thyroid cancer.
5. **Question:** How is thyromegaly diagnosed?
**Answer:** Thyromegaly is typically diagnosed through a physical examination, followed by imaging studies such as thyroid ultrasound. Blood tests to measure thyroid hormone levels (TSH, T4, and T3) are also essential.
6. **Question:** What is the role of iodine in thyromegaly?
**Answer:** Iodine deficiency is a major cause of thyromegaly in many parts of the world. Adequate iodine intake is essential for proper thyroid hormone production. Iodine supplementation can help prevent and treat thyromegaly in iodine-deficient areas.
7. **Question:** How is thyromegaly treated?
**Answer:** The treatment of thyromegaly depends on the underlying cause. Treatment options may include medication (e.g., thyroid hormone replacement for hypothyroidism, anti-thyroid drugs for hyperthyroidism), radioactive iodine therapy, or surgery.
8. **Question:** When is surgery necessary for thyromegaly?
**Answer:** Surgery may be necessary for thyromegaly if the enlargement is causing significant symptoms (e.g., difficulty breathing or swallowing), if there is suspicion of thyroid cancer, or if other treatments have failed.
9. **Question:** What is the prognosis for thyromegaly?
**Answer:** The prognosis for thyromegaly depends on the underlying cause and the effectiveness of treatment. In many cases, thyromegaly can be successfully managed with medication or surgery. However, long-term monitoring is often necessary to prevent recurrence or complications.
10. **Question:** Are there any lifestyle changes that can help manage thyromegaly?
**Answer:** While lifestyle changes cannot cure thyromegaly, they can help manage symptoms and improve overall health. These may include maintaining a healthy diet, avoiding smoking, and managing stress. It’s important to consult with a healthcare professional for personalized advice.
Conclusion & Strategic Call to Action
In summary, understanding thyromegaly, its underlying causes, and the appropriate ICD-10 codes is crucial for accurate diagnosis and effective management. Thyroid ultrasound plays a vital role in assessing thyromegaly and guiding further management decisions. Remember to consider the specific characteristics of the thyromegaly and any associated conditions when selecting the correct ICD-10 code. Leading experts in thyromegaly suggest that early detection and appropriate treatment can significantly improve patient outcomes.
The future of thyromegaly management may involve more personalized approaches based on genetic and molecular markers. Stay informed about the latest advances in thyroid research and clinical practice.
Share your experiences with thyromegaly ICD-10 coding in the comments below. Contact our experts for a consultation on thyromegaly management and coding best practices.
