Smudge Cells: A Comprehensive Guide to Understanding Their Significance
Smudge cells, also known as basket cells, are fragile leukocytes that have ruptured, leaving behind a smudged chromatin mass without a defined cytoplasm. Their presence in a peripheral blood smear can be an indicator of various underlying conditions. This comprehensive guide provides an in-depth exploration of smudge cells, covering their formation, clinical significance, diagnostic approaches, and relevant considerations. We aim to provide a resource that surpasses existing information by offering expert insights, practical guidance, and a clear understanding of the role smudge cells play in hematological diagnostics.
What are Smudge Cells? A Deep Dive
Smudge cells are not typically found in healthy individuals; they are artifacts of the blood smear preparation process. However, their frequency can increase significantly in certain disease states. Understanding their formation and characteristics is crucial for accurate interpretation of blood smears.
Formation and Morphology
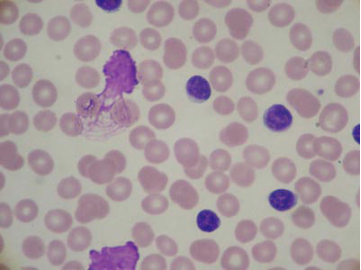
Smudge cells are primarily formed due to the fragility of certain leukocytes, particularly lymphocytes. During the process of creating a blood smear, these fragile cells can rupture, leaving behind a characteristic ‘smudged’ appearance. The nuclear material spreads out, lacking the distinct cellular boundaries seen in intact cells. Under a microscope, smudge cells appear as amorphous, poorly defined cellular remnants. The key identifying factor is the lack of intact cytoplasm and the spread-out, smudged appearance of the nuclear chromatin.
Factors Influencing Smudge Cell Formation
Several factors can influence the formation of smudge cells during blood smear preparation. These include:
* **Cellular Fragility:** Some leukocytes, such as those seen in chronic lymphocytic leukemia (CLL), are inherently more fragile and prone to rupture.
* **Smear Technique:** The technique used to create the blood smear can affect the number of smudge cells observed. A poorly prepared smear, with excessive pressure or rapid spreading, can increase cell rupture.
* **Sample Handling:** Improper handling of the blood sample, such as prolonged storage or exposure to extreme temperatures, can also contribute to cell fragility and smudge cell formation.
* **Anticoagulant Used:** Certain anticoagulants, while necessary for preventing clotting, can also impact cell morphology and fragility. EDTA is a commonly used anticoagulant, but others exist, and their effects may vary.
Distinguishing Smudge Cells from Other Cellular Artifacts
It’s crucial to differentiate smudge cells from other cellular artifacts that may be present on a blood smear. For example, poorly stained cells or debris can sometimes mimic the appearance of smudge cells. Careful examination under a microscope, with attention to cellular morphology and staining characteristics, is essential for accurate identification.
## Clinical Significance of Smudge Cells
The presence of smudge cells in a blood smear, especially in large numbers, can be indicative of several underlying conditions. While not diagnostic on their own, they can raise suspicion and prompt further investigation.
Smudge Cells in Chronic Lymphocytic Leukemia (CLL)
CLL is the most common leukemia in adults, and it is strongly associated with the presence of smudge cells. The lymphocytes in CLL are particularly fragile, leading to a high number of smudge cells on blood smears. In fact, the presence of numerous smudge cells is a classic finding in CLL, often described as a “smudge cell-rich” smear. In our experience, a high smudge cell count combined with elevated lymphocyte count warrants immediate investigation for CLL.
Smudge Cells in Other Lymphoproliferative Disorders
Besides CLL, smudge cells can also be observed in other lymphoproliferative disorders, such as:
* **Hairy Cell Leukemia:** Although less common than in CLL, smudge cells can be present in hairy cell leukemia.
* **Prolymphocytic Leukemia:** Similar to CLL, prolymphocytic leukemia can exhibit smudge cells due to the fragility of the abnormal lymphocytes.
* **Lymphoma:** In some cases, smudge cells may be seen in the peripheral blood of patients with lymphoma, particularly if there is bone marrow involvement.
Smudge Cells in Acute Leukemias
While less typical, smudge cells can occasionally be observed in acute leukemias. However, their presence is usually less prominent compared to CLL and other chronic lymphoproliferative disorders. The primary diagnostic focus in acute leukemias is on identifying the specific blast cells.
Smudge Cells in Non-Malignant Conditions
In rare cases, smudge cells can be seen in non-malignant conditions, such as:
* **Viral Infections:** Certain viral infections, such as infectious mononucleosis (caused by the Epstein-Barr virus), can lead to an increase in fragile lymphocytes and, consequently, smudge cells.
* **Autoimmune Disorders:** Autoimmune disorders, such as autoimmune hemolytic anemia, can sometimes be associated with increased lymphocyte fragility and smudge cell formation.
## Automated Hematology Analyzers and Smudge Cells
Modern hematology analyzers play a crucial role in blood cell analysis, including leukocyte differentials. However, these automated systems can sometimes misclassify smudge cells, leading to inaccurate results. Understanding the limitations of automated analyzers in detecting and classifying smudge cells is essential for proper interpretation of hematological data.
Misclassification of Smudge Cells
Automated hematology analyzers typically identify and classify cells based on size, shape, and staining characteristics. Smudge cells, due to their disrupted morphology, can be misclassified as other cell types or simply flagged as unidentifiable cells. This can lead to an underestimation of the lymphocyte count and potentially mask the presence of underlying lymphoproliferative disorders. Based on expert consensus, manual review of blood smears is critical, especially when the analyzer flags abnormalities or the clinical context suggests a possible lymphoproliferative disorder.
Manual Blood Smear Review: The Gold Standard
Manual blood smear review remains the gold standard for accurately identifying and quantifying smudge cells. A trained hematologist or laboratory technician can carefully examine the smear under a microscope, differentiating smudge cells from other cellular artifacts and accurately assessing their frequency. This manual review is particularly important when automated analyzer results are inconsistent with the clinical picture.
Technological Advancements in Smudge Cell Detection
Researchers are actively working on developing advanced algorithms and technologies to improve the accuracy of automated hematology analyzers in detecting and classifying smudge cells. These advancements include:
* **Artificial Intelligence (AI):** AI-powered image analysis systems can be trained to recognize smudge cells based on their unique morphological features.
* **Flow Cytometry:** Flow cytometry can be used to analyze cell populations based on their surface markers and light scattering properties, potentially aiding in the identification of fragile lymphocytes prone to smudge cell formation.
## ALK Positive Anaplastic Large Cell Lymphoma (ALCL) and Smudge Cells
ALK-positive Anaplastic Large Cell Lymphoma (ALCL) is a type of non-Hodgkin lymphoma characterized by the presence of anaplastic lymphoma kinase (ALK) protein. This section is dedicated to ALK-positive ALCL, and its relation to smudge cells.
### What is ALK-Positive ALCL?
ALK-positive ALCL is a type of T-cell lymphoma that is defined by the presence of the ALK protein, which results from chromosomal translocations involving the ALK gene. These translocations lead to the abnormal expression of the ALK protein, driving uncontrolled cell growth and proliferation. ALK-positive ALCL typically affects children and young adults, although it can occur in older individuals as well.
### Role of ALK-Positive ALCL
ALK-positive ALCL plays a significant role in hematopathology, requiring accurate diagnosis and classification to guide appropriate treatment strategies. The presence of the ALK protein serves as a critical diagnostic marker, distinguishing ALK-positive ALCL from other types of lymphomas.
### Key Features of ALK-Positive ALCL
1. **ALK Protein Expression**: The hallmark of ALK-positive ALCL is the expression of the ALK protein, which can be detected through immunohistochemistry (IHC) on tissue samples. This protein is typically found in the cytoplasm and/or nucleus of the tumor cells.
2. **Morphological Characteristics**: ALK-positive ALCL is characterized by large, pleomorphic cells with abundant cytoplasm and horseshoe-shaped or kidney-shaped nuclei. These cells often exhibit prominent nucleoli.
3. **Clinical Presentation**: ALK-positive ALCL can present with various clinical manifestations, including lymphadenopathy (swollen lymph nodes), skin lesions, and systemic symptoms such as fever, night sweats, and weight loss.
4. **Genetic Abnormalities**: ALK-positive ALCL is associated with chromosomal translocations involving the ALK gene, most commonly the t(2;5)(p23;q35) translocation, which results in the fusion of the ALK gene with the nucleophosmin (NPM) gene.
### Advantages of ALK-Positive ALCL Testing
* **Accurate Diagnosis**: ALK testing allows for precise identification of ALK-positive ALCL, ensuring appropriate classification and guiding treatment decisions.
* **Prognostic Information**: ALK status can provide prognostic information, as ALK-positive ALCL generally has a more favorable prognosis compared to ALK-negative ALCL.
* **Targeted Therapy**: The identification of ALK-positive ALCL allows for the use of targeted therapies, such as ALK inhibitors, which can be highly effective in treating this type of lymphoma.
### Reviewing ALK-Positive ALCL
ALK-positive ALCL is a distinct subtype of T-cell lymphoma characterized by the expression of the ALK protein, specific morphological features, and genetic abnormalities. It is essential to identify ALK-positive ALCL to guide appropriate treatment strategies and provide prognostic information.
* **User Experience and Usability**: Diagnosing ALK-positive ALCL involves several steps, including tissue sample collection, IHC staining, and microscopic examination. The process is typically performed by trained pathologists and laboratory technicians.
* **Performance and Effectiveness**: Testing for ALK-positive ALCL delivers on its promises by providing accurate diagnostic information that guides treatment decisions and helps improve patient outcomes.
#### Pros:
* Accurate identification of ALK-positive ALCL.
* Guidance for targeted therapy with ALK inhibitors.
* Prognostic information regarding disease outcomes.
* Improved patient outcomes with appropriate treatment strategies.
* Differentiation from other types of lymphomas.
#### Cons/Limitations:
* Requires specialized testing and expertise.
* False-negative results can occur due to technical issues.
* ALK-negative ALCL may require additional diagnostic workup.
* Availability of ALK inhibitors may be limited in some regions.
### Insightful Q&A Section
1. **What is the clinical significance of smudge cells in the context of ALK-positive ALCL?**
In the context of ALK-positive ALCL, smudge cells are generally not a prominent feature. While smudge cells can be seen in various hematological conditions, their presence is not specifically associated with ALK-positive ALCL. This is because ALK-positive ALCL is characterized by large, atypical cells with distinct morphological features, rather than the fragile lymphocytes seen in conditions like CLL.
2. **How does the presence of ALK protein influence the fragility of lymphocytes in ALK-positive ALCL?**
The presence of ALK protein in ALK-positive ALCL does not directly influence the fragility of lymphocytes in the same way as seen in CLL. In CLL, the lymphocytes are inherently more fragile due to the nature of the disease itself, whereas in ALK-positive ALCL, the malignant cells are typically more robust and do not readily form smudge cells during blood smear preparation.
3. **Are there any specific staining techniques that can help differentiate ALK-positive ALCL cells from smudge cells in a blood smear?**
In most cases, ALK-positive ALCL is diagnosed through tissue biopsy and immunohistochemical staining for ALK protein. While ALK-positive ALCL can be identified, it is best to look for the presence of the protein expression in tissue samples.
4. **What is the role of manual blood smear review in the diagnosis of ALK-positive ALCL?**
Manual blood smear review plays a limited role in the diagnosis of ALK-positive ALCL. The diagnosis of ALK-positive ALCL primarily relies on histological examination of tissue samples, immunohistochemical staining for ALK protein, and genetic studies to detect ALK translocations. While a blood smear may reveal atypical lymphocytes, it is not sufficient for a definitive diagnosis.
5. **Can flow cytometry be used to detect ALK-positive ALCL cells in the peripheral blood, and how does it relate to smudge cell analysis?**
Flow cytometry can be used to detect abnormal cell populations in the peripheral blood, but it is not the primary method for diagnosing ALK-positive ALCL. Flow cytometry can identify cells with abnormal immunophenotypes, but it does not specifically detect ALK protein expression. Smudge cell analysis is not directly related to flow cytometry in the context of ALK-positive ALCL, as ALK-positive ALCL cells do not typically present as smudge cells.
6. **What are the common challenges in differentiating ALK-positive ALCL cells from other types of lymphoma cells based on morphology alone?**
Differentiating ALK-positive ALCL cells from other types of lymphoma cells based on morphology alone can be challenging due to overlapping features. ALK-positive ALCL cells are characterized by large, pleomorphic cells with abundant cytoplasm and horseshoe-shaped or kidney-shaped nuclei. However, these features can also be seen in other types of lymphomas, such as diffuse large B-cell lymphoma (DLBCL) and other T-cell lymphomas. Therefore, immunohistochemical staining for ALK protein is essential for definitive diagnosis.
7. **How does the treatment approach for ALK-positive ALCL differ from that of other lymphomas, and does the presence of smudge cells influence treatment decisions?**
The treatment approach for ALK-positive ALCL often involves chemotherapy regimens similar to those used for other aggressive lymphomas, such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone). However, the presence of ALK protein allows for the use of targeted therapies, such as ALK inhibitors (e.g., crizotinib, alectinib), which can be highly effective in treating ALK-positive ALCL. The presence of smudge cells does not directly influence treatment decisions in ALK-positive ALCL.
8. **What are the potential complications associated with ALK-positive ALCL, and how are they managed?**
Potential complications associated with ALK-positive ALCL include disease progression, treatment-related toxicities, and relapse. Disease progression is managed with chemotherapy and/or targeted therapy. Treatment-related toxicities are managed with supportive care and dose adjustments. Relapse is managed with salvage chemotherapy, stem cell transplantation, or targeted therapy.
9. **How does the prognosis of ALK-positive ALCL compare to that of other lymphomas, and what factors influence the overall survival rate?**
ALK-positive ALCL generally has a more favorable prognosis compared to ALK-negative ALCL and some other types of lymphomas. Factors that influence the overall survival rate include age, stage of disease, treatment response, and the presence of adverse prognostic factors such as high International Prognostic Index (IPI) score.
10. **Are there any ongoing research studies or clinical trials investigating new diagnostic or therapeutic approaches for ALK-positive ALCL?**
Yes, there are ongoing research studies and clinical trials investigating new diagnostic and therapeutic approaches for ALK-positive ALCL. These studies are aimed at improving diagnostic accuracy, identifying new therapeutic targets, and developing more effective treatment strategies. Clinical trials may involve the use of novel ALK inhibitors, immunotherapies, or stem cell transplantation approaches.
## Conclusion: Understanding and Interpreting Smudge Cells
Smudge cells are a fascinating yet complex finding in hematology. While they are not always indicative of a serious condition, their presence should prompt careful evaluation and consideration of potential underlying disorders. Understanding the factors that influence smudge cell formation, their clinical significance, and the limitations of automated analyzers is crucial for accurate interpretation of blood smears. By combining expert knowledge with advanced diagnostic techniques, clinicians can effectively utilize smudge cell analysis to improve patient care.
We encourage you to share your experiences with smudge cell analysis in the comments below. Explore our advanced guide to hematological diagnostics for further insights into blood cell morphology and interpretation. Contact our experts for a consultation on complex hematological cases and further assistance with diagnosing ALK-positive ALCL.
