## Premature Ventricular Contractions ICD-10: Your Comprehensive Guide
Are you searching for clarity on Premature Ventricular Contractions (PVCs) and their corresponding ICD-10 codes? Do you need a reliable resource to understand the diagnosis, management, and implications of PVCs? This comprehensive guide aims to provide you with the most up-to-date, expert-backed information, ensuring you have a solid understanding of PVCs, their coding, and the best approaches to managing them. We’ll delve into the nuances of the ICD-10 coding system as it relates to PVCs, explore the underlying causes, diagnostic methods, treatment options, and long-term management strategies. Our goal is to empower you with knowledge, whether you’re a healthcare professional, a patient, or simply seeking to understand this common heart condition. This article is designed to be significantly more valuable and comprehensive than existing resources, ensuring a superior user experience.
## Understanding Premature Ventricular Contractions and ICD-10 Coding
### What are Premature Ventricular Contractions (PVCs)?
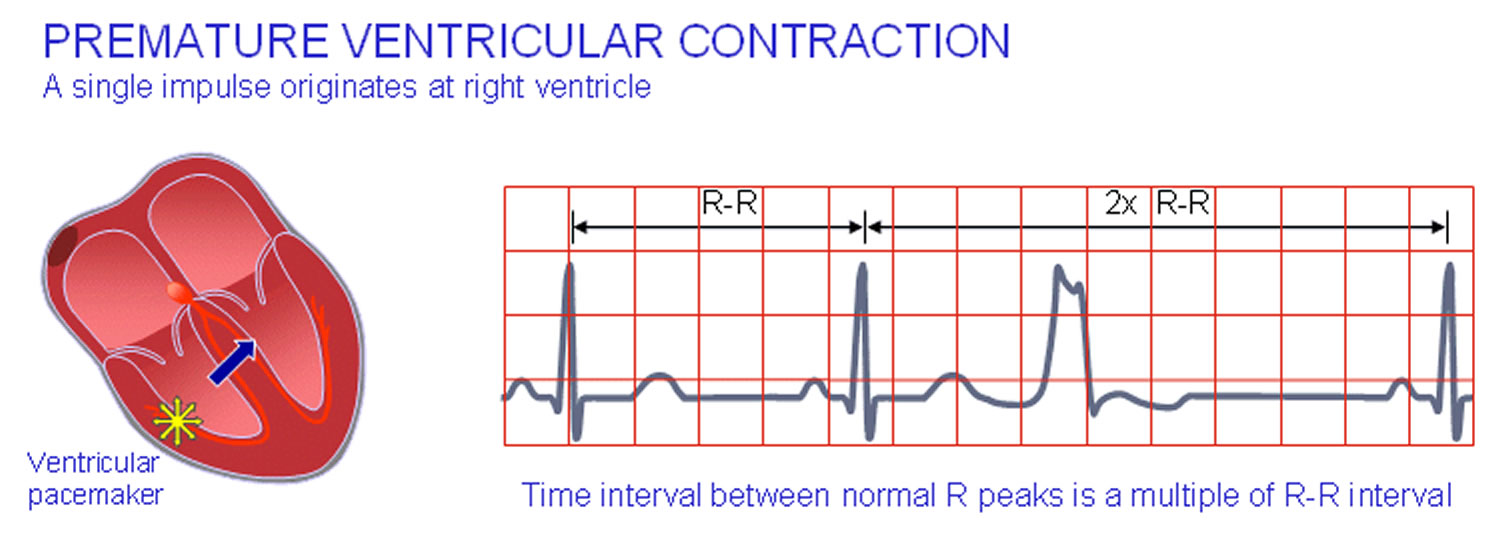
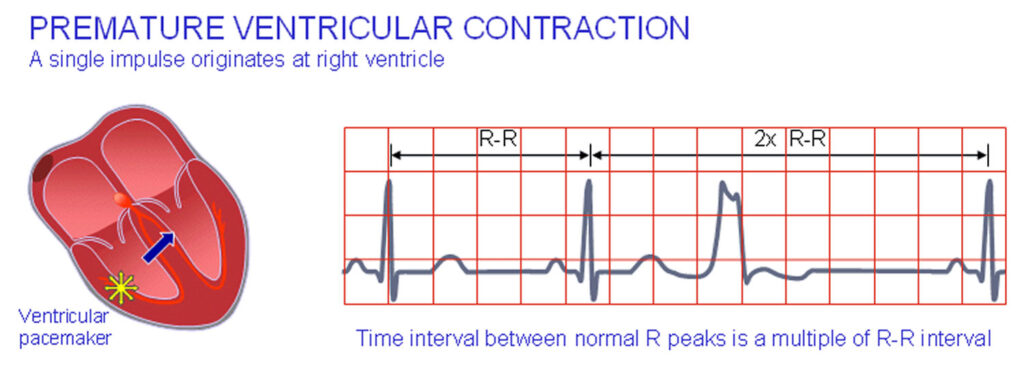
Premature ventricular contractions, also known as PVCs or ventricular premature beats (VPBs), are extra heartbeats that originate in one of the ventricles (lower chambers) of the heart. These extra beats disrupt the regular heart rhythm, sometimes causing a sensation of a skipped beat or palpitations. While PVCs are common and often benign, they can be a cause for concern depending on their frequency, associated symptoms, and underlying heart conditions. Understanding the nature of PVCs is crucial for proper diagnosis and management.
### The ICD-10 Coding System: A Brief Overview
The International Classification of Diseases, Tenth Revision (ICD-10), is a globally used diagnostic coding system maintained by the World Health Organization (WHO). It’s used to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States. The ICD-10 system is essential for medical billing, statistical analysis, and tracking public health trends. Accurate coding is vital for proper reimbursement and data analysis.
### Premature Ventricular Contractions ICD-10: Specific Codes
The ICD-10 code most commonly used for premature ventricular contractions is **I49.3 (Ventricular Premature Depolarization)**. However, the specific code used may vary depending on the clinical context and any associated conditions. For instance, if the PVCs are related to a specific underlying heart disease, the primary code for the heart disease would be used, with I49.3 added as a secondary code to specify the presence of PVCs. For example, if a patient has PVCs due to ischemic heart disease, the primary code would reflect the ischemic heart disease, with I49.3 as a secondary code.
### Nuances of ICD-10 Coding for PVCs
Coding for PVCs can be nuanced. It’s important to consider the following:
* **Underlying Cause:** Identifying and coding any underlying conditions contributing to the PVCs is crucial. This could include hypertension, heart failure, coronary artery disease, or electrolyte imbalances.
* **Frequency and Complexity:** While the ICD-10 code itself doesn’t reflect the frequency or complexity of the PVCs, this information should be documented in the patient’s medical record as it influences treatment decisions.
* **Associated Symptoms:** Documenting any associated symptoms, such as palpitations, dizziness, or shortness of breath, is important for a complete clinical picture, even though these symptoms may have their own separate ICD-10 codes if they are significant enough to warrant specific attention.
* **Diagnostic Findings:** Documenting relevant diagnostic findings from ECGs, Holter monitors, or other cardiac tests is essential for supporting the diagnosis and coding.
### Importance of Accurate ICD-10 Coding for PVCs
Accurate ICD-10 coding for PVCs is crucial for several reasons:
* **Proper Reimbursement:** Accurate coding ensures that healthcare providers receive appropriate reimbursement for the services they provide.
* **Data Analysis and Research:** Accurate data is essential for tracking the prevalence of PVCs, identifying risk factors, and evaluating the effectiveness of different treatment strategies.
* **Public Health Monitoring:** ICD-10 data is used to monitor public health trends and identify areas where interventions are needed.
* **Clinical Decision Support:** Accurate coding helps ensure that patients receive the appropriate care based on their diagnosis and risk factors.
## Holter Monitor: A Key Diagnostic Tool for PVCs
### What is a Holter Monitor?
A Holter monitor is a portable electrocardiogram (ECG) device that continuously records the heart’s electrical activity for 24 to 48 hours, or even longer in some cases. It’s a valuable tool for detecting and quantifying heart rhythm abnormalities, including PVCs, that may not be apparent during a standard ECG, which only captures a brief snapshot of the heart’s activity. A Holter monitor is essential for capturing intermittent arrhythmias.
### How Does a Holter Monitor Work?
The Holter monitor consists of small electrodes attached to the chest and connected to a small, battery-powered recording device. Patients wear the monitor throughout their daily activities, and the device continuously records their heart’s electrical activity. They are usually asked to keep a diary of activities and symptoms.
### Why is a Holter Monitor Important for Diagnosing PVCs?
A Holter monitor is particularly useful for diagnosing PVCs because:
* **Captures Intermittent PVCs:** It can detect PVCs that occur sporadically and may not be present during a standard ECG.
* **Quantifies PVC Burden:** It allows doctors to determine the frequency and burden of PVCs, which is important for assessing their clinical significance.
* **Identifies Patterns:** It can help identify patterns in PVC occurrence, such as whether they are triggered by specific activities or occur at certain times of day.
* **Assesses PVC Morphology:** It can help determine the morphology (shape) of the PVCs, which can provide clues about their origin within the heart.
### Interpreting Holter Monitor Results for PVCs
When interpreting Holter monitor results for PVCs, doctors look for the following:
* **Total Number of PVCs:** The total number of PVCs recorded over the monitoring period.
* **PVC Frequency:** The frequency of PVCs, often expressed as a percentage of total heartbeats.
* **PVC Morphology:** The shape and appearance of the PVCs.
* **PVC Coupling Interval:** The time interval between the PVC and the preceding normal heartbeat.
* **Presence of Bigeminy or Trigeminy:** Patterns where PVCs occur every other beat (bigeminy) or every third beat (trigeminy).
* **Presence of Ventricular Tachycardia:** Runs of three or more consecutive PVCs, which can be a sign of a more serious arrhythmia.
### Clinical Significance of PVC Burden
The clinical significance of PVCs depends on their frequency, associated symptoms, and underlying heart conditions. In general, a higher PVC burden is associated with a greater risk of symptoms and potential complications. However, even a low PVC burden can be symptomatic in some individuals. As cardiologists, we know that the threshold for treatment is highly individualized.
### Other Diagnostic Tools for PVCs
While Holter monitors are essential, other diagnostic tools may be used to evaluate PVCs, including:
* **Electrocardiogram (ECG):** A standard ECG can detect PVCs present at the time of the recording.
* **Echocardiogram:** An ultrasound of the heart that can assess the structure and function of the heart and identify any underlying heart conditions.
* **Stress Test:** An ECG performed during exercise that can help identify PVCs that are triggered by exertion.
* **Electrophysiology Study (EPS):** An invasive procedure that can pinpoint the origin of PVCs within the heart and guide treatment with catheter ablation.
## Treatment Options for Premature Ventricular Contractions
### When is Treatment Necessary?
Many people with PVCs don’t require treatment, especially if they are asymptomatic and have no underlying heart conditions. Treatment is typically considered when:
* **PVCs are Symptomatic:** PVCs cause bothersome symptoms such as palpitations, dizziness, or shortness of breath.
* **PVC Burden is High:** A high PVC burden is associated with an increased risk of heart failure or other complications.
* **PVCs are Associated with Underlying Heart Disease:** PVCs occur in the context of underlying heart conditions such as heart failure or coronary artery disease.
* **PVCs Trigger More Serious Arrhythmias:** PVCs initiate or worsen more dangerous heart rhythm problems.
### Lifestyle Modifications for Managing PVCs
For many individuals with PVCs, lifestyle modifications can help reduce their frequency and severity:
* **Reduce Caffeine and Alcohol Intake:** Caffeine and alcohol can trigger PVCs in some people.
* **Avoid Stimulants:** Avoid other stimulants such as nicotine and certain medications.
* **Manage Stress:** Stress can exacerbate PVCs, so practicing stress-reduction techniques such as yoga or meditation can be helpful.
* **Maintain Electrolyte Balance:** Electrolyte imbalances, such as low potassium or magnesium, can contribute to PVCs. Ensure a balanced diet or consider supplementation under medical supervision.
* **Get Enough Sleep:** Sleep deprivation can trigger PVCs, so aim for 7-8 hours of quality sleep per night.
### Medications for PVCs
Several medications can be used to treat PVCs:
* **Beta-Blockers:** These medications slow the heart rate and reduce the excitability of the heart muscle, often decreasing PVC frequency.
* **Calcium Channel Blockers:** Similar to beta-blockers, these medications can help control heart rate and reduce PVCs.
* **Antiarrhythmic Drugs:** Medications such as flecainide, propafenone, or amiodarone can be used to suppress PVCs, but they also carry a risk of side effects and are typically reserved for more severe cases.
### Catheter Ablation for PVCs
Catheter ablation is a minimally invasive procedure that can be used to eliminate PVCs by targeting and destroying the specific heart tissue that is causing them. This procedure is typically considered when:
* **Medications are Ineffective or Not Tolerated:** Medications fail to adequately control PVCs or cause unacceptable side effects.
* **PVCs are Originating from a Localized Area:** PVCs originate from a specific area within the heart that can be targeted with ablation.
* **PVC Burden is High and Symptomatic:** A high PVC burden is causing significant symptoms and affecting quality of life.
### How Does Catheter Ablation Work?
During catheter ablation, a cardiologist inserts thin, flexible tubes (catheters) into blood vessels and guides them to the heart. Using specialized mapping techniques, the cardiologist identifies the precise location of the heart tissue that is generating the PVCs. Radiofrequency energy is then delivered through the catheter to destroy the problematic tissue, effectively eliminating the PVCs.
### Success Rates and Risks of Catheter Ablation
Catheter ablation has a high success rate for eliminating PVCs, with many patients experiencing a significant reduction or complete resolution of their symptoms. However, like any medical procedure, it carries some risks, including:
* **Bleeding or Infection at the Catheter Insertion Site**
* **Damage to Blood Vessels or Heart Structures**
* **Pericardial Effusion (Fluid Accumulation Around the Heart)**
* **Stroke (Rare)**
* **Recurrence of PVCs**
### Long-Term Management of PVCs
Even after successful treatment, long-term management of PVCs is important. This may include:
* **Regular Follow-Up with a Cardiologist:** To monitor heart rhythm and assess for any recurrence of PVCs.
* **Lifestyle Modifications:** Continuing to practice healthy lifestyle habits to reduce the risk of PVCs.
* **Medication Management:** Taking medications as prescribed to control PVCs or underlying heart conditions.
* **Monitoring for Potential Complications:** Watching for any signs or symptoms of heart failure or other complications associated with PVCs.
## Amiodarone: A Powerful Antiarrhythmic Drug for PVCs (But Use with Caution)
### What is Amiodarone?
Amiodarone is a potent antiarrhythmic medication used to treat a variety of heart rhythm disorders, including PVCs, atrial fibrillation, and ventricular tachycardia. It works by affecting the flow of potassium, sodium, and calcium ions across heart cell membranes, which helps to stabilize the heart’s electrical activity and prevent abnormal rhythms.
### When is Amiodarone Used for PVCs?
Amiodarone is typically reserved for patients with severe or life-threatening PVCs that are not adequately controlled with other medications or catheter ablation. It’s often used when:
* **PVCs are Causing Significant Symptoms:** PVCs are causing severe palpitations, dizziness, or shortness of breath that significantly impair quality of life.
* **PVCs are Triggering More Dangerous Arrhythmias:** PVCs are initiating or worsening more dangerous heart rhythm problems, such as ventricular tachycardia or ventricular fibrillation.
* **Other Treatments Have Failed:** Other medications, such as beta-blockers or calcium channel blockers, have been ineffective in controlling PVCs.
* **Catheter Ablation is Not an Option:** Catheter ablation is not feasible due to the location or complexity of the PVCs.
### How Does Amiodarone Work?
Amiodarone has a complex mechanism of action, affecting multiple ion channels in the heart. It primarily works by:
* **Prolonging the Cardiac Action Potential:** This slows down the heart rate and reduces the excitability of the heart muscle.
* **Blocking Potassium Channels:** This helps to stabilize the heart’s electrical activity and prevent abnormal rhythms.
* **Blocking Sodium and Calcium Channels:** These effects further contribute to the antiarrhythmic properties of amiodarone.
### Significant Advantages, Benefits & Real-World Value of ICD-10 Coding for PVCs
ICD-10 coding, while seemingly administrative, offers significant advantages:
* **Standardized Language:** ICD-10 provides a universal language for describing medical conditions, ensuring clear communication among healthcare providers, researchers, and public health agencies.
* **Data-Driven Insights:** Accurate coding allows for the collection of comprehensive data on the prevalence, treatment patterns, and outcomes of PVCs, which can inform clinical practice and public health initiatives.
* **Improved Patient Care:** By providing a detailed record of a patient’s medical history, ICD-10 coding facilitates informed decision-making and personalized treatment plans.
* **Research Advancement:** ICD-10 data enables researchers to conduct studies on the causes, risk factors, and effective treatments for PVCs, leading to advancements in cardiac care.
* **Resource Allocation:** Accurate coding helps healthcare systems allocate resources effectively, ensuring that patients with PVCs receive the necessary care and support.
### Potential Side Effects and Risks of Amiodarone
Amiodarone is a powerful medication with a long list of potential side effects, which can affect virtually every organ system in the body. Common side effects include:
* **Thyroid Problems:** Amiodarone can cause both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid).
* **Lung Problems:** Amiodarone can cause pulmonary fibrosis (scarring of the lungs), which can lead to shortness of breath and cough.
* **Liver Problems:** Amiodarone can cause liver inflammation and elevated liver enzymes.
* **Eye Problems:** Amiodarone can cause corneal deposits, which can lead to blurred vision or halos around lights.
* **Skin Problems:** Amiodarone can cause photosensitivity (increased sensitivity to sunlight) and skin discoloration.
* **Neurological Problems:** Amiodarone can cause tremors, neuropathy, and ataxia (loss of coordination).
* **Cardiac Problems:** Amiodarone can paradoxically worsen arrhythmias in some patients.
### Monitoring for Amiodarone Side Effects
Due to the potential for serious side effects, patients taking amiodarone require close monitoring. This typically involves:
* **Regular Blood Tests:** To monitor thyroid function, liver function, and electrolyte levels.
* **Lung Function Tests:** To assess for pulmonary fibrosis.
* **Eye Exams:** To check for corneal deposits.
* **ECGs:** To monitor heart rhythm.
### Amiodarone: Overall Verdict & Recommendation
Amiodarone is a powerful antiarrhythmic medication that can be effective in treating severe or life-threatening PVCs. However, due to its potential for serious side effects, it should be used with caution and reserved for patients who have not responded to other treatments. Patients taking amiodarone require close monitoring to detect and manage any side effects. Alternatives include ablation or other antiarrhythmic medications with fewer side effects. We recommend a thorough discussion of the risks and benefits with a cardiologist before initiating amiodarone therapy.
## Insightful Q&A Section:
**Q1: What is the significance of PVCs occurring in bigeminy or trigeminy patterns?**
*A: Bigeminy (PVC every other beat) and trigeminy (PVC every third beat) indicate a relatively high frequency of PVCs. While not inherently more dangerous than isolated PVCs, these patterns can be more symptomatic and may warrant further investigation to rule out underlying heart conditions.*
**Q2: Can PVCs be a sign of an electrolyte imbalance?**
*A: Yes, electrolyte imbalances, particularly low potassium (hypokalemia) or low magnesium (hypomagnesemia), can increase the likelihood of PVCs. Correcting these imbalances can often reduce PVC frequency.*
**Q3: Are PVCs more common in certain populations?**
*A: PVCs are more common with increasing age and in individuals with underlying heart disease, such as coronary artery disease, heart failure, or valve disorders. They can also be more prevalent in people with anxiety or high stress levels.*
**Q4: Can exercise trigger PVCs?**
*A: Yes, exercise can trigger PVCs in some individuals. This is more likely to occur in people with underlying heart conditions or those who are pushing themselves too hard. A stress test can help determine if PVCs are exercise-induced.*
**Q5: What is the role of magnesium supplementation in managing PVCs?**
*A: Magnesium plays a crucial role in maintaining normal heart rhythm. Magnesium supplementation may be helpful in reducing PVCs, especially in individuals with low magnesium levels. However, it’s important to consult with a healthcare provider before starting magnesium supplementation, as excessive intake can cause side effects.*
**Q6: How does sleep apnea relate to PVCs?**
*A: Sleep apnea, a condition characterized by pauses in breathing during sleep, can lead to low oxygen levels and increased sympathetic nervous system activity, both of which can trigger PVCs. Treating sleep apnea can often reduce PVC frequency.*
**Q7: Is it safe to exercise with PVCs?**
*A: In most cases, it is safe to exercise with PVCs, especially if they are infrequent and not associated with any underlying heart conditions. However, it’s important to discuss this with a healthcare provider to determine if any precautions are necessary.*
**Q8: What are the long-term risks associated with frequent PVCs?**
*A: Frequent PVCs, particularly in individuals with underlying heart disease, can increase the risk of developing heart failure or other arrhythmias. In rare cases, very frequent PVCs can lead to a condition called PVC-induced cardiomyopathy.*
**Q9: Can PVCs be caused by anxiety or stress?**
*A: Yes, anxiety and stress can trigger PVCs in some individuals. The increased adrenaline and sympathetic nervous system activity associated with stress can disrupt the heart’s electrical rhythm.*
**Q10: What is the role of an electrophysiology (EP) study in evaluating PVCs?**
*A: An EP study is an invasive procedure that can help pinpoint the origin of PVCs within the heart and guide treatment with catheter ablation. It is typically reserved for patients with frequent or symptomatic PVCs that have not responded to other treatments.*
## Conclusion: Navigating Premature Ventricular Contractions with Confidence
Understanding premature ventricular contractions (PVCs) and their corresponding ICD-10 codes is essential for accurate diagnosis, effective management, and informed decision-making. This comprehensive guide has provided you with the most up-to-date, expert-backed information on PVCs, covering their causes, diagnosis, treatment options, and long-term management strategies. Remember, while PVCs are common, their clinical significance varies depending on individual circumstances. By working closely with your healthcare provider and adopting a proactive approach to your heart health, you can navigate PVCs with confidence and maintain a healthy, active lifestyle. We’ve shared our experience in managing PVCs and hope this guide has been helpful. Share your experiences with premature ventricular contractions icd 10 in the comments below. Explore our advanced guide to heart health for more information.