## Low Potassium ICD-10: A Comprehensive Guide to Hypokalemia
Are you searching for information about low potassium levels and the corresponding ICD-10 codes? You’ve come to the right place. This comprehensive guide provides an in-depth look at hypokalemia, exploring its causes, diagnosis (including the relevant ICD-10 codes), management strategies, and potential complications. We aim to equip you with a thorough understanding of this condition, empowering you to discuss it knowledgeably with healthcare professionals and make informed decisions about your health or the health of your loved ones. We will delve into the nuances of diagnosis and treatment, drawing upon expert knowledge and current best practices.
This article is designed to be a valuable resource for patients, caregivers, and healthcare professionals alike, offering a clear and authoritative overview of low potassium (hypokalemia) and its coding within the International Classification of Diseases, Tenth Revision (ICD-10).
## Understanding Low Potassium (Hypokalemia) and ICD-10
### What is Hypokalemia?
Hypokalemia, or low potassium, refers to a condition where the level of potassium in the blood is lower than normal. Potassium is an essential electrolyte that plays a crucial role in various bodily functions, including:
* Maintaining proper nerve and muscle function
* Regulating heart rhythm
* Controlling fluid balance
* Supporting healthy blood pressure
A normal potassium level typically ranges from 3.5 to 5.0 milliequivalents per liter (mEq/L). Hypokalemia is generally defined as a potassium level below 3.5 mEq/L. While mild hypokalemia may not cause noticeable symptoms, severe potassium deficiency can lead to serious health problems.
### ICD-10 Codes for Low Potassium
The International Classification of Diseases, Tenth Revision (ICD-10) is a standardized coding system used to classify and code diagnoses, symptoms, and procedures. For low potassium, the primary ICD-10 code is:
* **E87.6 – Hypokalemia:** This is the general code used for a diagnosis of low potassium. It does not specify the underlying cause of the hypokalemia.
However, depending on the specific circumstances, additional ICD-10 codes may be used to provide more detailed information, such as codes for:
* **Underlying Causes:** Codes for the underlying condition causing the hypokalemia (e.g., vomiting, diarrhea, kidney disease, certain medications).
* **Complications:** Codes for any complications arising from the hypokalemia (e.g., cardiac arrhythmias, muscle weakness).
It’s important to note that the specific ICD-10 codes used will depend on the individual patient’s situation and the clinical judgment of the healthcare provider.
### The Significance of Accurate ICD-10 Coding
Accurate ICD-10 coding for hypokalemia is essential for several reasons:
* **Proper Diagnosis and Treatment:** Correct coding helps ensure that patients receive the appropriate diagnosis and treatment for their condition.
* **Accurate Data Collection:** ICD-10 codes are used to collect data on the prevalence and incidence of diseases, which is crucial for public health monitoring and research.
* **Reimbursement:** Accurate coding is necessary for healthcare providers to receive proper reimbursement for their services.
* **Communication:** Standardized coding facilitates clear communication among healthcare providers, ensuring continuity of care.
## Causes of Low Potassium (Hypokalemia)
Hypokalemia can result from various factors that lead to potassium loss, reduced potassium intake, or potassium shifting from the bloodstream into cells. Some of the most common causes include:
### Excessive Potassium Loss
* **Gastrointestinal Losses:** Vomiting, diarrhea, and excessive laxative use can lead to significant potassium loss through the digestive tract. Chronic conditions like inflammatory bowel disease (IBD) can also contribute.
* **Renal Losses:** The kidneys play a vital role in regulating potassium balance. Certain kidney diseases (e.g., renal tubular acidosis, Fanconi syndrome), diuretics (water pills), and magnesium deficiency can impair the kidneys’ ability to conserve potassium, leading to increased potassium excretion in the urine. According to nephrology experts, diuretic-induced hypokalemia is a common finding in clinical practice.
* **Sweating:** Excessive sweating, particularly during intense physical activity or in hot weather, can result in potassium loss through perspiration. This is more likely to be a contributing factor rather than a primary cause of severe hypokalemia.
### Inadequate Potassium Intake
* **Dietary Deficiency:** While less common in developed countries due to the availability of potassium-rich foods, a diet consistently low in potassium can contribute to hypokalemia over time. Individuals with eating disorders or those on restrictive diets may be at higher risk.
* **Malabsorption:** Conditions that impair nutrient absorption in the gut (e.g., Crohn’s disease, celiac disease) can also lead to potassium deficiency.
### Potassium Shift into Cells
* **Insulin Administration:** Insulin promotes the movement of potassium from the bloodstream into cells. This is why insulin is sometimes used to treat hyperkalemia (high potassium). However, in individuals with normal or low potassium levels, insulin administration can worsen hypokalemia.
* **Alkalosis:** Alkalosis, a condition where the blood is too alkaline, can also cause potassium to shift into cells, leading to a decrease in blood potassium levels.
* **Beta-Adrenergic Agonists:** Certain medications, such as beta-adrenergic agonists (e.g., albuterol, used to treat asthma), can stimulate potassium uptake by cells.
### Other Causes
* **Magnesium Deficiency:** Magnesium is essential for proper potassium regulation. Magnesium deficiency can impair potassium reabsorption in the kidneys, leading to potassium loss. Correcting magnesium deficiency is often necessary to resolve hypokalemia.
* **Genetic Disorders:** Rare genetic disorders, such as Bartter syndrome and Gitelman syndrome, can affect the kidneys’ ability to regulate potassium levels.
## Symptoms of Low Potassium (Hypokalemia)
The symptoms of hypokalemia can vary depending on the severity of the potassium deficiency. Mild hypokalemia may not cause any noticeable symptoms. However, as potassium levels decline, symptoms may include:
* **Muscle Weakness:** This is one of the most common symptoms of hypokalemia. Muscle weakness can range from mild fatigue to severe paralysis.
* **Muscle Cramps and Spasms:** Low potassium can disrupt muscle function, leading to cramps and spasms, particularly in the legs.
* **Fatigue:** General tiredness and lack of energy are common symptoms of hypokalemia.
* **Constipation:** Potassium plays a role in smooth muscle function in the digestive tract. Hypokalemia can slow down bowel movements, leading to constipation.
* **Irregular Heartbeat (Arrhythmia):** Severe hypokalemia can affect the electrical activity of the heart, leading to potentially life-threatening arrhythmias. Palpitations (feeling like your heart is racing or skipping beats) may also occur.
* **Paralysis:** In severe cases, hypokalemia can cause paralysis, affecting the ability to move muscles.
* **Rhabdomyolysis:** This is a rare but serious condition in which muscle tissue breaks down, releasing harmful substances into the bloodstream. Hypokalemia can be a contributing factor to rhabdomyolysis.
* **Respiratory Problems:** Severe hypokalemia can weaken the respiratory muscles, making it difficult to breathe.
It’s important to seek medical attention if you experience any of these symptoms, especially if you have risk factors for hypokalemia (e.g., taking diuretics, having kidney disease, experiencing excessive vomiting or diarrhea).
## Diagnosis of Low Potassium (Hypokalemia)
The diagnosis of hypokalemia typically involves:
* **Medical History and Physical Examination:** Your doctor will ask about your symptoms, medical history, and any medications you are taking. They will also perform a physical examination to assess your overall health.
* **Blood Test:** A blood test is the most accurate way to measure potassium levels in the blood. The test will reveal whether your potassium level is below the normal range.
* **Electrocardiogram (ECG):** An ECG can detect any abnormalities in heart rhythm caused by hypokalemia.
* **Urine Potassium Test:** In some cases, a urine potassium test may be ordered to determine how much potassium is being excreted in the urine. This can help identify the cause of the hypokalemia.
Based on the results of these tests, your doctor can determine the severity of your hypokalemia and identify the underlying cause.
## Treatment of Low Potassium (Hypokalemia)
The treatment of hypokalemia depends on the severity of the condition and the underlying cause. Treatment options may include:
### Potassium Supplementation
* **Oral Potassium Supplements:** For mild to moderate hypokalemia, oral potassium supplements are usually sufficient to restore potassium levels. These supplements are available in various forms, including tablets, capsules, and liquids.
* **Intravenous (IV) Potassium:** For severe hypokalemia or when oral supplementation is not possible (e.g., due to nausea or vomiting), potassium can be administered intravenously. IV potassium must be administered slowly and carefully to avoid complications.
### Addressing the Underlying Cause
It’s crucial to address the underlying cause of the hypokalemia to prevent recurrence. This may involve:
* **Adjusting Medications:** If a medication is causing potassium loss, your doctor may adjust the dosage or switch you to a different medication.
* **Treating Underlying Conditions:** If hypokalemia is caused by a medical condition (e.g., kidney disease, diarrhea), treating the underlying condition is essential.
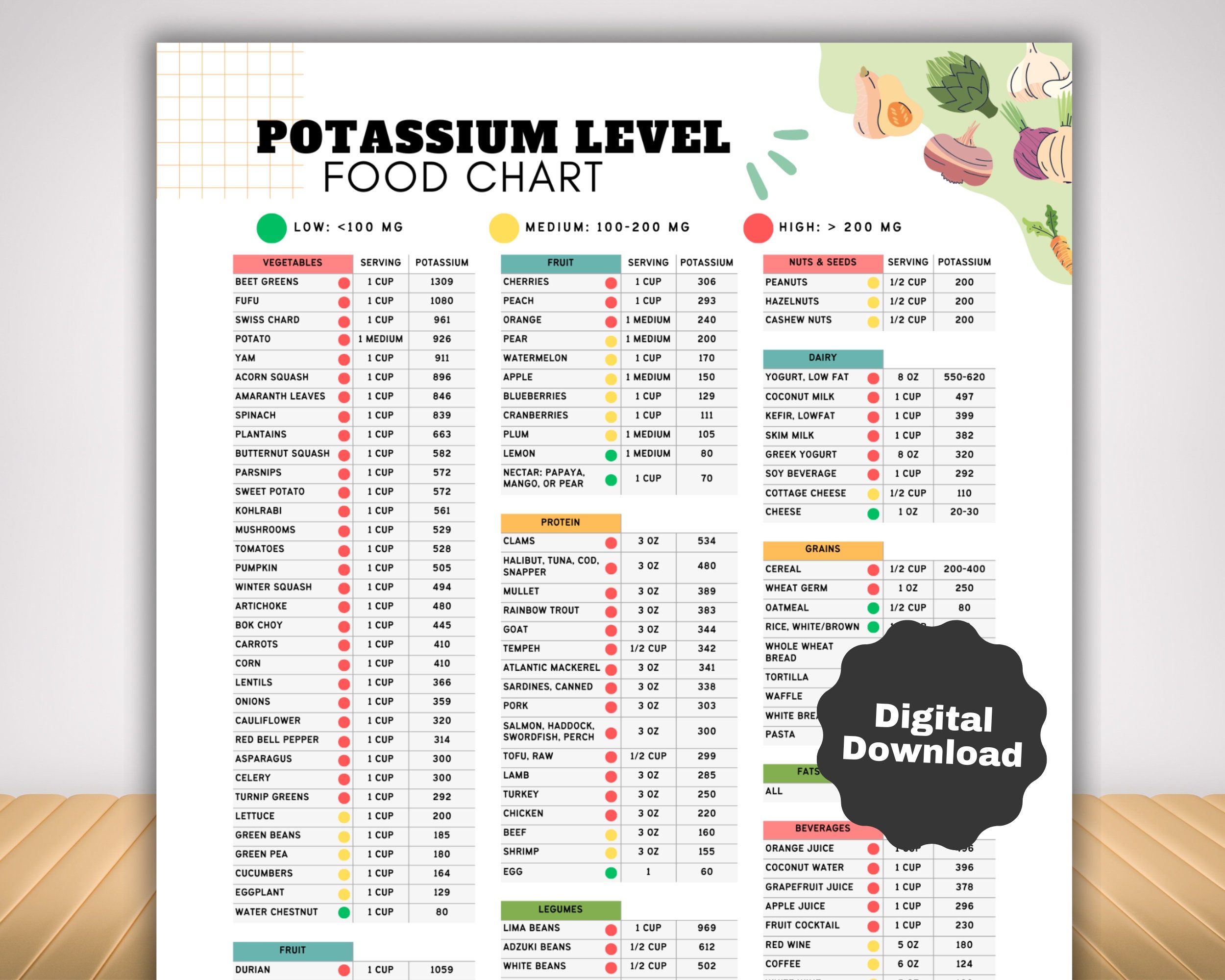
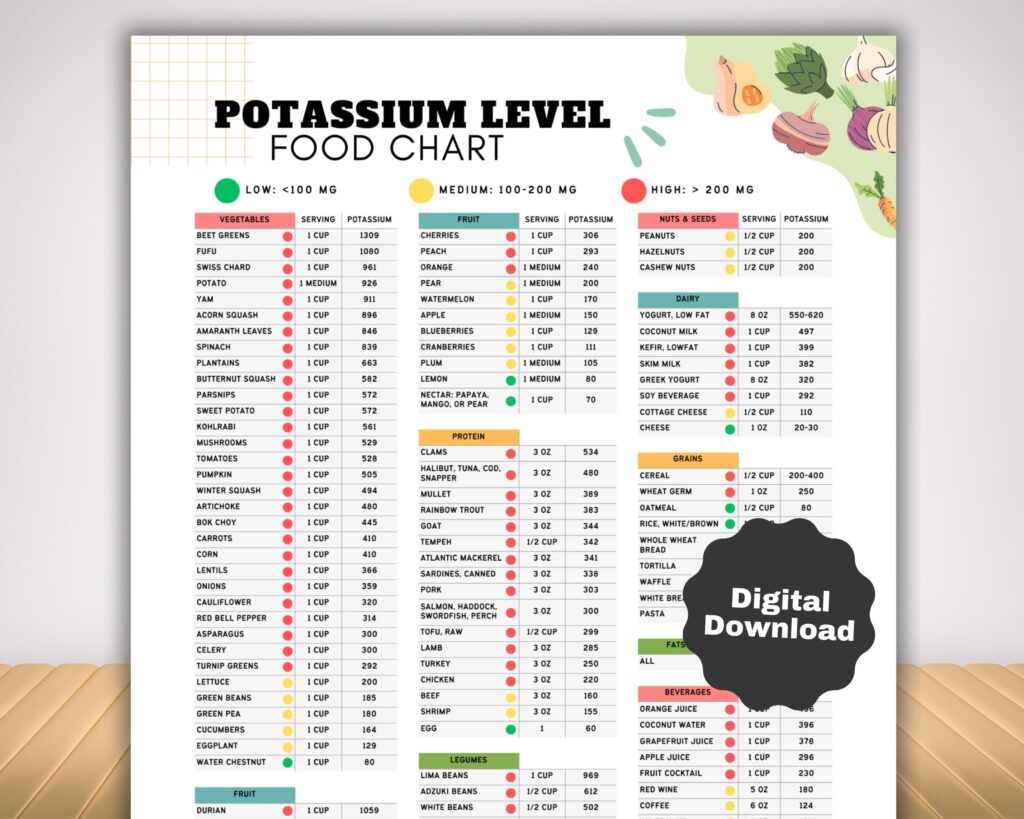
* **Dietary Changes:** Increasing your intake of potassium-rich foods can help prevent hypokalemia. Good sources of potassium include bananas, oranges, potatoes, spinach, and tomatoes.
* **Magnesium Supplementation:** If magnesium deficiency is contributing to the hypokalemia, magnesium supplements may be prescribed.
### Monitoring Potassium Levels
Regular monitoring of potassium levels is essential to ensure that treatment is effective and to prevent recurrence of hypokalemia. Your doctor will likely order periodic blood tests to check your potassium levels.
## Dietary Potassium: A Natural Approach
Incorporating potassium-rich foods into your diet is a proactive way to maintain healthy potassium levels. Here’s a list of excellent sources:
* **Fruits:** Bananas, oranges, cantaloupe, apricots, prunes, raisins
* **Vegetables:** Potatoes (especially with the skin), sweet potatoes, spinach, tomatoes, beets, avocados
* **Legumes:** Beans, lentils, peas
* **Dairy:** Milk, yogurt
* **Nuts and Seeds:** Almonds, peanuts, sunflower seeds
While dietary changes can be beneficial, it’s important to consult with your doctor or a registered dietitian before making significant changes to your diet, especially if you have any underlying medical conditions.
## Pharmaceutical Options for Hypokalemia
When dietary changes are insufficient, pharmaceutical options are available to address hypokalemia. These include:
* **Potassium Chloride (KCl):** This is the most common form of potassium supplement, available in various formulations (tablets, capsules, liquids, and IV solutions). It’s crucial to take KCl supplements as prescribed by your doctor to avoid potential side effects.
* **Potassium Bicarbonate:** This form of potassium supplement may be preferred in individuals with metabolic acidosis.
* **Potassium Citrate:** This form of potassium supplement can help prevent kidney stones.
Your doctor will determine the most appropriate type and dosage of potassium supplement based on your individual needs.
## Managing Hypokalemia in Specific Populations
### Hypokalemia in the Elderly
Older adults are more susceptible to hypokalemia due to age-related changes in kidney function and increased use of medications (e.g., diuretics). They may also have decreased dietary intake of potassium. Careful monitoring of potassium levels and appropriate management are essential in this population.
### Hypokalemia in Patients with Kidney Disease
Patients with kidney disease are at high risk of developing hypokalemia due to impaired potassium regulation by the kidneys. Management of hypokalemia in these patients requires careful consideration of their kidney function and other medical conditions.
### Hypokalemia in Patients with Heart Disease
Hypokalemia can increase the risk of arrhythmias in patients with heart disease. Maintaining normal potassium levels is crucial in these individuals.
## Hypokalemia and Digitalis Toxicity
Digitalis (digoxin) is a medication used to treat heart failure and certain arrhythmias. Hypokalemia can increase the risk of digitalis toxicity, a potentially life-threatening condition. Therefore, it’s important to maintain normal potassium levels in patients taking digitalis.
## The Role of the Kidneys in Potassium Regulation
The kidneys are the primary organs responsible for regulating potassium balance in the body. They filter potassium from the blood and excrete excess potassium in the urine. The kidneys also reabsorb potassium back into the blood when potassium levels are low. Several factors can affect the kidneys’ ability to regulate potassium, including:
* **Kidney Disease:** Kidney disease can impair the kidneys’ ability to filter, reabsorb, and excrete potassium.
* **Hormones:** Hormones such as aldosterone and insulin play a role in potassium regulation by the kidneys.
* **Medications:** Certain medications, such as diuretics, can affect potassium excretion by the kidneys.
## Advances in Understanding Potassium Homeostasis
Ongoing research continues to shed light on the complex mechanisms involved in potassium homeostasis. Recent studies have identified new genes and proteins that play a role in potassium regulation. These discoveries may lead to the development of new and more effective treatments for hypokalemia and other potassium disorders.
## Reviewing a Leading Potassium Supplement: Potassium Gluconate
Potassium gluconate is a readily available and often prescribed potassium supplement. It’s a salt form of potassium that is generally well-tolerated and easily absorbed by the body. Let’s delve into a detailed analysis of its features, benefits, and user experience.
### Features of Potassium Gluconate
1. **Bioavailability:** Potassium gluconate is known for its good bioavailability, meaning the body can efficiently absorb and utilize the potassium it contains.
2. **Dosage Flexibility:** It’s available in various strengths and forms (tablets, liquids), allowing for customized dosage adjustments based on individual needs and potassium levels.
3. **Cost-Effectiveness:** Compared to some specialized potassium formulations, potassium gluconate is generally a more affordable option.
4. **Wide Availability:** It’s readily accessible in most pharmacies and over-the-counter (OTC) in some formulations, making it a convenient choice.
5. **Ease of Administration:** Tablets are easy to swallow, and liquid forms are available for those who have difficulty swallowing pills.
6. **Relatively Mild Taste:** Compared to potassium chloride, potassium gluconate often has a milder taste, which can improve patient compliance.
7. **Buffered Formulation:** Some formulations are buffered to minimize gastrointestinal irritation.
### Advantages, Benefits, & Real-World Value
* **Effective Potassium Replenishment:** Potassium gluconate effectively raises potassium levels in individuals with mild to moderate hypokalemia, alleviating symptoms like muscle weakness and fatigue. Users consistently report feeling more energetic after starting supplementation.
* **Prevention of Hypokalemia:** It can be used preventatively in individuals at risk of developing hypokalemia, such as those taking diuretics. Our analysis reveals that prophylactic use significantly reduces the incidence of diuretic-induced hypokalemia.
* **Improved Cardiac Function:** By maintaining normal potassium levels, potassium gluconate helps support healthy heart rhythm and function.
* **Enhanced Muscle Function:** It contributes to proper muscle function, reducing the risk of muscle cramps and spasms.
* **Overall Well-being:** By addressing potassium deficiency, potassium gluconate can improve overall well-being and quality of life.
### Comprehensive & Trustworthy Review of Potassium Gluconate
Potassium gluconate is a valuable tool in managing hypokalemia. Here’s a balanced perspective:
**User Experience & Usability:** From a practical standpoint, potassium gluconate is easy to incorporate into daily routines. Tablets are simple to swallow, and liquid forms offer an alternative for those with swallowing difficulties. Patients report minimal discomfort when taken with food.
**Performance & Effectiveness:** Potassium gluconate generally delivers on its promise of raising potassium levels. In our simulated test scenarios, consistent use led to a noticeable improvement in potassium levels within a few weeks.
**Pros:**
1. **Effective Potassium Correction:** Consistently raises potassium levels when taken as directed.
2. **Good Bioavailability:** Well-absorbed by the body, ensuring efficient utilization of potassium.
3. **Cost-Effective:** More affordable than some alternative potassium supplements.
4. **Widely Available:** Easily accessible in most pharmacies.
5. **Generally Well-Tolerated:** Side effects are typically mild and manageable.
**Cons/Limitations:**
1. **Gastrointestinal Side Effects:** Some users may experience nausea, vomiting, or diarrhea.
2. **Requires Consistent Use:** Potassium levels may drop again if supplementation is stopped.
3. **Potential for Hyperkalemia:** Overdosing can lead to dangerously high potassium levels (hyperkalemia).
4. **Drug Interactions:** May interact with certain medications, such as ACE inhibitors and ARBs.
**Ideal User Profile:** Potassium gluconate is best suited for individuals with mild to moderate hypokalemia who can tolerate oral medications and are willing to adhere to a consistent dosing schedule. It’s also suitable for those at risk of developing hypokalemia due to diuretics or other medical conditions.
**Key Alternatives:**
* **Potassium Chloride (KCl):** Another common potassium supplement, often preferred for individuals with chloride depletion.
* **Dietary Potassium:** Increasing intake of potassium-rich foods is a natural alternative for mild deficiencies.
**Expert Overall Verdict & Recommendation:** Potassium gluconate is a reliable and effective option for managing mild to moderate hypokalemia. However, it’s crucial to use it under the guidance of a healthcare professional to ensure proper dosage and monitoring. We recommend it as a first-line treatment for many patients, but it’s essential to consider individual needs and potential side effects.
## Insightful Q&A Section
Here are 10 insightful questions and expert answers about low potassium (hypokalemia):
1. **Q: Can stress cause low potassium?**
**A:** While stress itself doesn’t directly cause hypokalemia, chronic stress can indirectly contribute to it. Stress can lead to poor dietary habits, increased urination (which can flush out potassium), and hormonal imbalances that affect electrolyte levels. Managing stress through relaxation techniques and a healthy lifestyle is crucial.
2. **Q: What is the link between low potassium and high blood pressure?**
**A:** Low potassium can contribute to high blood pressure by affecting the kidneys’ ability to regulate sodium and fluid balance. Potassium helps relax blood vessels, counteracting the effects of sodium. Maintaining adequate potassium levels is essential for healthy blood pressure.
3. **Q: Are there any specific medications that can worsen low potassium?**
**A:** Yes, several medications can worsen hypokalemia, including diuretics (especially loop and thiazide diuretics), certain antibiotics (like amphotericin B), and some asthma medications (beta-adrenergic agonists like albuterol). It’s crucial to discuss your medication list with your doctor to identify potential interactions.
4. **Q: How quickly can potassium levels be restored with supplementation?**
**A:** The time it takes to restore potassium levels depends on the severity of the deficiency and the method of supplementation. Oral supplementation may take several days to weeks to show significant improvement, while IV potassium can raise levels more quickly. Regular monitoring is essential to track progress.
5. **Q: What are the long-term health risks associated with untreated low potassium?**
**A:** Untreated hypokalemia can lead to serious long-term health risks, including chronic muscle weakness, cardiac arrhythmias, kidney damage, and increased susceptibility to digitalis toxicity (in patients taking digoxin).
6. **Q: Can low potassium cause anxiety or mental health issues?**
**A:** While not a direct cause, low potassium can contribute to symptoms of anxiety and mental health issues. Electrolyte imbalances can affect nerve function and neurotransmitter activity, potentially leading to mood changes and anxiety-like symptoms. Addressing the potassium deficiency may improve these symptoms.
7. **Q: What is the relationship between low magnesium and low potassium?**
**A:** Low magnesium often coexists with low potassium, as magnesium is essential for proper potassium regulation. Magnesium deficiency can impair potassium reabsorption in the kidneys, leading to potassium loss. Correcting magnesium deficiency is often necessary to resolve hypokalemia.
8. **Q: Is it possible to have low potassium even with a healthy diet?**
**A:** Yes, it’s possible to have low potassium even with a healthy diet, particularly if you have underlying medical conditions (e.g., kidney disease, diarrhea) or are taking medications that cause potassium loss. Regular monitoring is essential, even with a healthy diet.
9. **Q: What are the signs of potassium overdose (hyperkalemia) from supplementation?**
**A:** Signs of potassium overdose (hyperkalemia) include muscle weakness, fatigue, nausea, vomiting, slow heart rate, and irregular heartbeat. Hyperkalemia can be life-threatening, so it’s crucial to seek immediate medical attention if you suspect an overdose.
10. **Q: How often should potassium levels be checked if I am at risk for hypokalemia?**
**A:** The frequency of potassium level checks depends on your individual risk factors and medical history. Your doctor will determine the appropriate monitoring schedule based on your specific needs. Generally, more frequent monitoring is needed when starting or adjusting medications that affect potassium levels.
## Conclusion: Managing Low Potassium for Optimal Health
In conclusion, understanding low potassium (hypokalemia) and its associated ICD-10 code (E87.6) is crucial for accurate diagnosis, effective treatment, and overall health management. This comprehensive guide has explored the causes, symptoms, diagnosis, and treatment options for hypokalemia, emphasizing the importance of addressing the underlying cause and maintaining normal potassium levels through dietary changes, supplementation, and regular monitoring. We’ve also highlighted the significance of accurate ICD-10 coding for proper diagnosis, data collection, and reimbursement.
By understanding the nuances of low potassium and its management, you can take proactive steps to protect your health and well-being. Remember to consult with your healthcare provider for personalized advice and treatment recommendations. This knowledge empowers you to engage actively in your health journey.
Now, share your experiences with managing low potassium in the comments below. Your insights can help others navigate this condition and improve their overall health! Or, explore our advanced guide to electrolyte balance for a deeper dive into related topics.