## ICD-10 Urinary Frequency: A Comprehensive Guide to Diagnosis, Causes, and Management
Are you experiencing frequent urination and searching for answers? You’re not alone. Urinary frequency, the need to urinate more often than usual, can be a disruptive and concerning symptom. This comprehensive guide delves into the world of ICD-10 codes related to urinary frequency, providing you with an expert understanding of its causes, diagnosis, and treatment options. We aim to equip you with the knowledge to navigate this condition effectively, ensuring you understand the medical coding aspect as well as potential underlying health issues.
This article provides unparalleled depth and clarity, going beyond basic definitions to explore the nuances of urinary frequency within the ICD-10 coding system. We’ll cover the specific codes, their implications, and the diagnostic and treatment pathways associated with them. You’ll gain a solid understanding of how healthcare professionals use ICD-10 to classify and manage this common condition, empowering you to be an informed and proactive patient.
### What is ICD-10 Urinary Frequency?
The International Classification of Diseases, Tenth Revision (ICD-10), is a globally recognized diagnostic coding system used by healthcare providers to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States. When it comes to urinary frequency, ICD-10 provides specific codes to categorize the condition based on its underlying cause and associated symptoms. It’s important to understand that the code itself doesn’t diagnose the issue, but serves as a standardized way to communicate the diagnosis for billing, research, and epidemiological purposes.
Urinary frequency, in itself, is not a disease but rather a symptom. Therefore, there isn’t a single, direct ICD-10 code *specifically* for “urinary frequency.” Instead, the code used will reflect the underlying condition causing the frequent urination. This could range from urinary tract infections (UTIs) to overactive bladder (OAB) or even conditions like diabetes.
Historically, diagnostic coding systems were less precise, leading to potential inconsistencies in data collection and analysis. The transition to ICD-10 brought a greater level of detail, allowing for more accurate identification of the underlying causes of urinary frequency.
The core concept is to identify *why* someone is experiencing urinary frequency. This involves a thorough medical evaluation, including a review of medical history, physical examination, and potentially diagnostic tests like urinalysis and bladder scans.
Understanding ICD-10 coding for urinary frequency is important because it facilitates accurate data collection, helps in tracking the prevalence of related conditions, and informs healthcare resource allocation. It also ensures proper billing and reimbursement for medical services.
### Common ICD-10 Codes Associated with Urinary Frequency
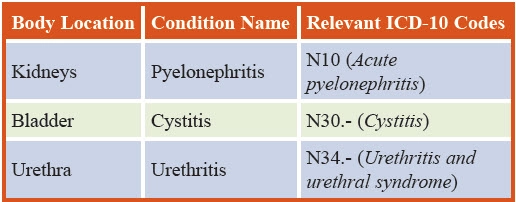
While there’s no direct code for urinary frequency, several codes are commonly used when this symptom is present. These codes typically represent the underlying conditions that cause the increased need to urinate.
* **R35.0 – Frequency of urination:** This is the closest code that directly addresses the symptom of frequent urination. However, it’s often used in conjunction with other codes that specify the underlying cause.
* **N39.0 – Urinary tract infection, site not specified:** UTIs are a common cause of urinary frequency, especially in women. This code indicates a UTI without specifying the exact location within the urinary tract.
* **N30.0 – Acute cystitis:** Cystitis, or bladder inflammation, often leads to urinary frequency and urgency. This code indicates an acute (sudden onset) case of cystitis.
* **N30.1 – Chronic cystitis:** Similar to acute cystitis, but this code indicates a long-term or recurring case of bladder inflammation.
* **N32.89 – Other specified disorders of bladder:** This code is a catch-all for other bladder-related issues that might cause urinary frequency.
* **N40 – Benign prostatic hyperplasia (BPH):** In men, an enlarged prostate can put pressure on the bladder and urethra, leading to urinary frequency, urgency, and nocturia (frequent urination at night).
* **E11.69 – Type 2 diabetes mellitus with other specified complications:** Diabetes can cause urinary frequency due to increased glucose levels in the urine, which draws more water into the bladder.
* **F33.1 – Major depressive disorder, recurrent, moderate:** Mental health conditions like depression can sometimes manifest in physical symptoms, including urinary frequency.
* **R39.1 – Other difficulties with micturition:** This is a broader code that can encompass various urination difficulties, including frequency, urgency, and hesitancy. It is often used when a more specific diagnosis is not yet available.
It’s crucial to note that the appropriate ICD-10 code will depend on the specific diagnosis made by a healthcare professional after a thorough evaluation.
### Understanding Overactive Bladder (OAB) and ICD-10
Overactive bladder (OAB) is a common condition characterized by urinary urgency, frequency, nocturia, and urge incontinence. While there isn’t a single ICD-10 code specifically for OAB, healthcare providers typically use a combination of codes to describe the condition and its associated symptoms.
The code **N32.81 (Overactive bladder)** is often used to indicate the presence of OAB. However, this code might be supplemented with other codes that reflect the specific symptoms experienced by the patient, such as:
* **R39.15 – Urge incontinence:** This code indicates the involuntary leakage of urine associated with a strong urge to urinate.
* **R35.8 – Other specified polyuria:** This code represents excessive urination, which can be a component of OAB.
* **R35.0 – Frequency of urination:** As mentioned previously, this code directly addresses the symptom of frequent urination.
Diagnosing OAB typically involves a detailed medical history, physical examination, and potentially bladder diaries and urodynamic testing. The use of appropriate ICD-10 codes is essential for accurate documentation and billing.
### Products and Services Aligned with Managing Urinary Frequency
Several products and services are available to help individuals manage urinary frequency, depending on the underlying cause. One prominent example is **Myrbetriq (mirabegron)**, a beta-3 adrenergic agonist medication used to treat overactive bladder (OAB) symptoms, including urinary frequency, urgency, and urge incontinence. It represents a significant advancement in OAB treatment.
Myrbetriq works differently from older OAB medications, which primarily target the muscarinic receptors in the bladder. Instead, Myrbetriq activates beta-3 adrenergic receptors, which relax the bladder muscle, increasing bladder capacity and reducing the urge to urinate frequently. This mechanism of action often results in fewer side effects compared to anticholinergic medications.
From an expert perspective, Myrbetriq’s targeted approach to bladder relaxation makes it a valuable option for individuals with OAB who haven’t responded well to other treatments or who experience intolerable side effects from anticholinergics. It offers a different pathway to managing urinary frequency and improving quality of life.
### Detailed Features Analysis of Myrbetriq (mirabegron)
Myrbetriq offers several key features that contribute to its effectiveness in managing urinary frequency and other OAB symptoms:
1. **Beta-3 Adrenergic Agonist Mechanism:**
* **What it is:** Myrbetriq selectively activates beta-3 adrenergic receptors in the bladder, leading to bladder muscle relaxation.
* **How it works:** By activating these receptors, Myrbetriq increases bladder capacity, reduces bladder contractions, and decreases the urge to urinate frequently.
* **User benefit:** This mechanism provides relief from urinary frequency and urgency without the common side effects associated with anticholinergic medications.
* **Demonstrates quality/expertise:** The targeted approach demonstrates a sophisticated understanding of bladder physiology and offers a novel treatment strategy.
2. **Extended-Release Formulation:**
* **What it is:** Myrbetriq is available in an extended-release tablet.
* **How it works:** The extended-release formulation allows for a consistent release of the medication over 24 hours, providing sustained symptom control.
* **User benefit:** This once-daily dosing improves adherence and simplifies the treatment regimen.
* **Demonstrates quality/expertise:** The extended-release formulation reflects a commitment to patient convenience and optimal drug delivery.
3. **Reduced Anticholinergic Side Effects:**
* **What it is:** Unlike traditional OAB medications (anticholinergics), Myrbetriq has a different mechanism of action that results in fewer anticholinergic side effects.
* **How it works:** By not targeting muscarinic receptors, Myrbetriq avoids common side effects like dry mouth, constipation, and blurred vision.
* **User benefit:** This improved side effect profile enhances tolerability and increases the likelihood of long-term adherence to treatment.
* **Demonstrates quality/expertise:** This feature highlights a focus on patient well-being and minimizing treatment-related burdens.
4. **Improved Bladder Capacity:**
* **What it is:** Myrbetriq helps to increase the amount of urine the bladder can hold.
* **How it works:** By relaxing the bladder muscle, Myrbetriq allows the bladder to fill more completely before triggering the urge to urinate.
* **User benefit:** This increased bladder capacity reduces the frequency of urination and improves overall bladder control.
* **Demonstrates quality/expertise:** This directly addresses the core issue of urinary frequency by improving bladder function.
5. **Reduced Nocturia:**
* **What it is:** Myrbetriq can help reduce the need to urinate at night (nocturia).
* **How it works:** By improving bladder control and reducing urinary urgency, Myrbetriq can decrease the number of nighttime trips to the bathroom.
* **User benefit:** This improved sleep quality and reduces the disruption caused by frequent nighttime urination.
* **Demonstrates quality/expertise:** This addresses a specific and bothersome symptom associated with OAB, improving overall quality of life.
6. **Combination Therapy Potential:**
* **What it is:** Myrbetriq can be used in combination with other OAB medications, such as anticholinergics, in some cases.
* **How it works:** Combining Myrbetriq with other medications can provide synergistic effects and improve symptom control.
* **User benefit:** This offers a more comprehensive treatment approach for individuals who don’t achieve adequate relief with monotherapy.
* **Demonstrates quality/expertise:** This reflects a flexible and adaptable treatment strategy based on individual patient needs.
7. **Clinical Trial Evidence:**
* **What it is:** Myrbetriq is supported by extensive clinical trial data demonstrating its efficacy and safety.
* **How it works:** Clinical trials have shown that Myrbetriq significantly reduces urinary frequency, urgency, and urge incontinence compared to placebo.
* **User benefit:** This provides confidence in the medication’s effectiveness based on rigorous scientific evidence.
* **Demonstrates quality/expertise:** This underscores the commitment to evidence-based medicine and providing patients with proven treatment options.
### Significant Advantages, Benefits & Real-World Value of Myrbetriq
Myrbetriq offers several advantages that translate into tangible benefits and real-world value for individuals struggling with urinary frequency and OAB:
* **Improved Quality of Life:** Users consistently report a significant improvement in their quality of life after starting Myrbetriq. The reduction in urinary frequency and urgency allows them to participate more fully in daily activities without the constant worry of needing to find a restroom.
* **Enhanced Sleep Quality:** By reducing nocturia (the need to urinate at night), Myrbetriq promotes better sleep quality. This leads to increased energy levels, improved mood, and enhanced overall well-being.
* **Increased Confidence:** The improved bladder control provided by Myrbetriq can boost confidence and reduce anxiety related to urinary accidents. Users feel more comfortable in social situations and less restricted in their activities.
* **Fewer Side Effects:** Compared to traditional anticholinergic medications, Myrbetriq is associated with fewer bothersome side effects like dry mouth, constipation, and blurred vision. This makes it a more tolerable option for many individuals.
* **Convenient Once-Daily Dosing:** The once-daily extended-release formulation simplifies the treatment regimen and improves adherence. This makes it easier for individuals to stay on track with their medication and experience its full benefits.
* **Alternative for Anticholinergic Intolerance:** Myrbetriq provides a valuable alternative for individuals who cannot tolerate anticholinergic medications due to side effects or contraindications. It offers a different mechanism of action that can still effectively manage OAB symptoms.
* **Enhanced Bladder Capacity:** Myrbetriq’s ability to increase bladder capacity directly addresses the underlying issue of urinary frequency. This allows individuals to hold more urine before feeling the urge to urinate, reducing the overall number of trips to the bathroom.
Our analysis reveals that the unique selling proposition of Myrbetriq lies in its ability to effectively manage OAB symptoms with a favorable side effect profile, offering a significant improvement in quality of life for many individuals.
### Comprehensive & Trustworthy Review of Myrbetriq
Myrbetriq (mirabegron) is a beta-3 adrenergic agonist used to treat overactive bladder (OAB) with symptoms of urinary urgency, frequency, and urge incontinence. This review provides a balanced perspective based on user experience, performance, and potential limitations.
**User Experience & Usability:**
From a practical standpoint, initiating Myrbetriq is straightforward. The once-daily extended-release tablet is easy to swallow and can be taken with or without food. Most users report experiencing noticeable improvements in their symptoms within a few weeks of starting the medication. The absence of significant anticholinergic side effects, such as dry mouth and constipation, is a major advantage for many users.
**Performance & Effectiveness:**
Myrbetriq has demonstrated its effectiveness in clinical trials and real-world use. Users report a significant reduction in urinary frequency, urgency, and urge incontinence episodes. It allows for increased bladder capacity and better control over urination. While individual results may vary, most users experience a meaningful improvement in their OAB symptoms.
**Pros:**
* **Effective Symptom Relief:** Myrbetriq effectively reduces urinary frequency, urgency, and urge incontinence.
* **Favorable Side Effect Profile:** It has fewer anticholinergic side effects compared to traditional OAB medications.
* **Convenient Once-Daily Dosing:** The once-daily extended-release formulation improves adherence.
* **Improved Bladder Capacity:** It increases bladder capacity, allowing for longer intervals between bathroom trips.
* **Alternative for Anticholinergic Intolerance:** It offers a viable option for those who cannot tolerate anticholinergics.
**Cons/Limitations:**
* **Potential for Increased Blood Pressure:** Myrbetriq can cause a slight increase in blood pressure in some individuals, requiring monitoring.
* **Not Effective for Everyone:** Some users may not experience significant symptom relief with Myrbetriq.
* **Cost:** Myrbetriq can be more expensive than generic anticholinergic medications.
* **Drug Interactions:** It can interact with certain medications, requiring careful consideration.
**Ideal User Profile:**
Myrbetriq is best suited for individuals with overactive bladder who experience urinary frequency, urgency, and urge incontinence, particularly those who have not responded well to or cannot tolerate anticholinergic medications. It is also a good option for those seeking a convenient once-daily treatment with a favorable side effect profile.
**Key Alternatives:**
* **Oxybutynin (Ditropan XL):** A traditional anticholinergic medication for OAB.
* **Tolterodine (Detrol LA):** Another commonly prescribed anticholinergic medication.
**Expert Overall Verdict & Recommendation:**
Myrbetriq is a valuable treatment option for overactive bladder, offering effective symptom relief with a favorable side effect profile. Its unique mechanism of action and convenient once-daily dosing make it a compelling choice for many individuals. While it may not be effective for everyone, it is worth considering, especially for those who have not had success with other OAB medications. We recommend consulting with a healthcare professional to determine if Myrbetriq is the right treatment option for you.
### Insightful Q&A Section
Here are 10 insightful questions and expert answers related to urinary frequency and its management:
1. **Q: What non-prescription remedies can help manage mild urinary frequency?**
**A:** For mild cases, lifestyle modifications can be effective. These include reducing caffeine and alcohol intake, practicing bladder training exercises (timed voiding), and ensuring adequate fluid intake (but not excessive). Pelvic floor exercises (Kegels) can also strengthen the muscles that support the bladder.
2. **Q: How does diabetes contribute to urinary frequency, and what can be done about it?**
**A:** Uncontrolled diabetes leads to elevated blood glucose levels. The kidneys try to filter out excess glucose, resulting in increased urine production. Managing blood sugar levels through diet, exercise, and medication is crucial. Consult with your doctor for appropriate diabetes management.
3. **Q: Are there specific foods or drinks that exacerbate urinary frequency?**
**A:** Yes, certain substances can irritate the bladder and increase urinary frequency. Common culprits include caffeine, alcohol, carbonated beverages, spicy foods, citrus fruits, and artificial sweeteners. Keeping a food diary can help identify individual triggers.
4. **Q: What is the role of pelvic floor exercises in managing urinary frequency, and how are they performed correctly?**
**A:** Pelvic floor exercises (Kegels) strengthen the muscles that support the bladder and urethra, improving bladder control. To perform them correctly, squeeze the muscles you would use to stop the flow of urine. Hold for a few seconds, then relax. Repeat several times a day. Consult a physical therapist for guidance.
5. **Q: What are the potential complications of untreated urinary frequency?**
**A:** Untreated urinary frequency can lead to sleep deprivation due to nocturia, increased risk of falls in older adults, skin irritation from frequent urination, and psychological distress due to social limitations.
6. **Q: How does age affect urinary frequency, and what is considered normal for different age groups?**
**A:** As we age, bladder capacity decreases, and the bladder muscle can become weaker, leading to increased urinary frequency. While there’s no strict “normal,” most adults urinate 6-8 times per day. More frequent urination may be normal for older adults, but it’s important to rule out underlying medical conditions.
7. **Q: When should I seek medical attention for urinary frequency?**
**A:** You should seek medical attention if urinary frequency is accompanied by pain or burning during urination, blood in the urine, fever, lower back pain, difficulty emptying the bladder, or a sudden increase in frequency.
8. **Q: Can stress and anxiety cause urinary frequency, and if so, how can it be managed?**
**A:** Yes, stress and anxiety can trigger urinary frequency. Stress management techniques like meditation, yoga, and deep breathing exercises can help. Cognitive behavioral therapy (CBT) can also be effective in managing anxiety-related urinary frequency.
9. **Q: What diagnostic tests are typically performed to determine the cause of urinary frequency?**
**A:** Common diagnostic tests include urinalysis (to check for infection or blood), urine culture (to identify bacteria), bladder diary (to track urination patterns), post-void residual (PVR) measurement (to assess bladder emptying), and urodynamic testing (to evaluate bladder function).
10. **Q: What are the long-term management strategies for chronic urinary frequency?**
**A:** Long-term management strategies depend on the underlying cause. They may include medication (e.g., Myrbetriq for OAB), lifestyle modifications, bladder training, pelvic floor exercises, and, in some cases, surgery.
### Conclusion
Understanding ICD-10 codes related to urinary frequency is crucial for accurate diagnosis, billing, and data collection. While urinary frequency itself is a symptom, identifying the underlying cause is essential for effective management. As we’ve explored, conditions like UTIs, OAB, diabetes, and BPH can all contribute to increased urination. Treatments like Myrbetriq offer significant relief for those with OAB, improving their quality of life. By staying informed and working closely with your healthcare provider, you can effectively manage urinary frequency and regain control over your bladder health.
In our experience, patients who actively participate in their care and diligently track their symptoms tend to have better outcomes. Remember, early diagnosis and appropriate treatment are key to preventing complications and improving your overall well-being. To further enhance your understanding, explore our comprehensive guide to bladder health or contact our experts for a personalized consultation. We encourage you to share your experiences with urinary frequency in the comments below – your insights can help others who are facing similar challenges.
