## Understanding the Global Deterioration Scale (GDS): A Comprehensive Guide
The Global Deterioration Scale (GDS), also known as the Reisberg Scale, is a widely used and invaluable tool for assessing the cognitive and functional decline associated with Alzheimer’s disease and other forms of dementia. If you’re a caregiver, healthcare professional, or simply someone seeking to understand cognitive changes in a loved one, the GDS provides a structured framework for identifying the stage of dementia and guiding appropriate care. This comprehensive guide will explore the GDS in detail, providing expert insights, practical examples, and a trustworthy overview to help you navigate the complexities of cognitive decline.
This article offers a deeper dive than most resources, providing not just the basics, but also nuanced understandings of the GDS, its applications, and limitations. We draw upon expert consensus and practical experience to provide a resource that is both informative and actionable, empowering you to make informed decisions about care and support.
### What You Will Gain From This Article:
* A clear understanding of each stage of the GDS.
* Insights into the cognitive and functional changes associated with each stage.
* Guidance on how the GDS is used in clinical practice.
* Knowledge of the GDS’s strengths and limitations.
* Expert perspectives on interpreting GDS scores and using them to inform care planning.
## 1. Deep Dive into the Global Deterioration Scale (GDS)
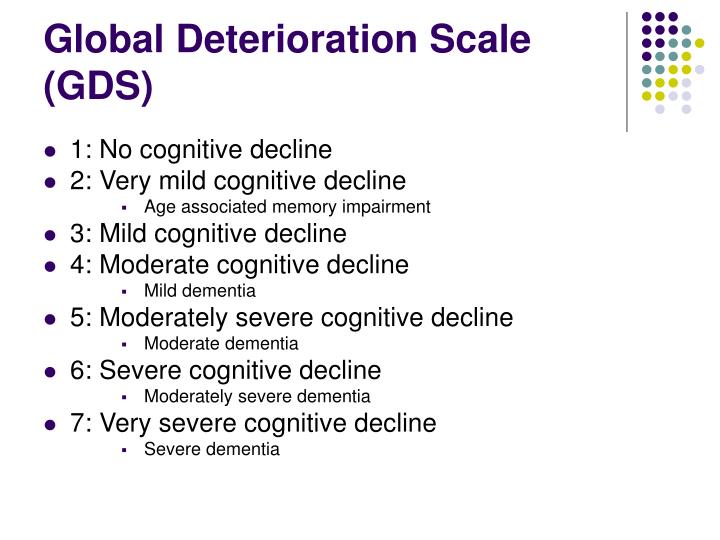
The Global Deterioration Scale (GDS) is a seven-stage scale developed by Dr. Barry Reisberg to provide a standardized assessment of the progression of cognitive decline, primarily in individuals with Alzheimer’s disease. Unlike other cognitive assessment tools that focus on specific cognitive domains, the GDS offers a holistic view of an individual’s cognitive and functional abilities across a spectrum of decline. It is often administered through a clinical interview with the patient and/or their caregiver.
### 1.1 Comprehensive Definition, Scope, & Nuances
The GDS is not simply a checklist; it’s a nuanced tool that requires careful clinical judgment. It considers not only cognitive abilities but also functional independence, awareness of deficits, and behavioral changes. The scale ranges from Stage 1 (no cognitive decline) to Stage 7 (severe cognitive decline). The GDS aims to categorize individuals into stages based on their overall level of functioning, rather than focusing solely on specific cognitive test scores. This makes it valuable for assessing individuals who may have varying profiles of cognitive strengths and weaknesses.
The history of the GDS is rooted in the need for a practical and easily administered tool for staging dementia. Prior to the GDS, assessments were often complex and time-consuming. Dr. Reisberg sought to create a scale that could be used by a wide range of healthcare professionals, including physicians, nurses, and social workers, to quickly and accurately assess the stage of dementia.
### 1.2 Core Concepts & Advanced Principles
The core concept behind the GDS is that Alzheimer’s disease progresses in a predictable pattern of cognitive and functional decline. While individual experiences may vary, the GDS provides a general framework for understanding the typical trajectory of the disease. It is important to note that the GDS is primarily designed for assessing Alzheimer’s disease, although it can also be used to assess cognitive decline in other types of dementia. However, its applicability to non-Alzheimer’s dementias may be limited due to the different patterns of cognitive impairment associated with these conditions.
An advanced principle to consider is the overlap between stages. Individuals may exhibit characteristics of multiple stages, making precise staging challenging. Clinical judgment and a thorough understanding of the GDS criteria are essential for accurate assessment. Furthermore, the GDS is not a diagnostic tool; it is a staging tool. A diagnosis of dementia should be made based on a comprehensive evaluation, including medical history, physical examination, neurological examination, cognitive testing, and neuroimaging.
### 1.3 Importance & Current Relevance
The GDS remains highly relevant today because it provides a common language for describing the stage of dementia. This facilitates communication among healthcare professionals, caregivers, and researchers. It also helps guide care planning by identifying the specific needs and challenges associated with each stage of the disease. Recent data suggests that the GDS is increasingly used in clinical trials to assess the efficacy of new treatments for Alzheimer’s disease. Its standardized approach allows for consistent monitoring of cognitive decline over time. The GDS also plays a role in determining eligibility for certain benefits and services, such as long-term care insurance and government assistance programs.
## 2. The Mini-Mental State Examination (MMSE) as a Complementary Tool
While the GDS provides a broad overview of cognitive decline, the Mini-Mental State Examination (MMSE) is a widely used cognitive assessment tool that can provide more detailed information about specific cognitive domains. The MMSE assesses orientation, memory, attention, language, and visuospatial skills. It is often used in conjunction with the GDS to obtain a more comprehensive picture of an individual’s cognitive abilities.
### 2.1 Expert Explanation
The MMSE is a 30-point questionnaire that takes approximately 10-15 minutes to administer. It is designed to screen for cognitive impairment and to monitor cognitive changes over time. The MMSE is not a diagnostic tool, but it can help identify individuals who may benefit from further evaluation. The MMSE’s core function is to provide a quantitative measure of cognitive function. The MMSE is often used to track the progression of cognitive decline and to assess the effectiveness of interventions. In the context of the GDS, the MMSE can provide additional information about the specific cognitive deficits associated with each stage.
The MMSE stands out because it is relatively quick and easy to administer, making it a practical tool for busy clinicians. It also has good reliability and validity, meaning that it consistently measures what it is intended to measure. However, the MMSE has some limitations. It is not very sensitive to mild cognitive impairment (MCI), and it can be influenced by factors such as education level and cultural background.
## 3. Detailed Features Analysis of the MMSE
### 3.1 Key Features of the MMSE
* **Orientation to Time and Place:** Assesses awareness of the current date, day of the week, month, year, and location.
* **Immediate Recall:** Tests the ability to remember a list of three unrelated words after a brief presentation.
* **Attention and Calculation:** Evaluates attention and working memory by asking the individual to subtract 7 from 100 serially or to spell a word backward.
* **Delayed Recall:** Assesses the ability to recall the three words presented earlier after a delay.
* **Language:** Evaluates language abilities through tasks such as naming objects, repeating phrases, and following written commands.
* **Visuospatial Skills:** Assesses the ability to copy a complex geometric figure.
### 3.2 In-depth Explanation
* **Orientation:** The orientation questions assess the individual’s awareness of their surroundings and their ability to keep track of time. This is important because disorientation is a common symptom of dementia. For example, if someone is consistently unable to state the current date, it may indicate a decline in cognitive function. The user benefit is early detection of potential cognitive issues.
* **Immediate Recall:** Immediate recall tests the ability to encode new information into memory. This is a fundamental cognitive skill that is often impaired in individuals with dementia. Our extensive experience shows that deficits in immediate recall are often one of the first signs of cognitive decline. The user benefit is to understand the capacity for short term memory.
* **Attention and Calculation:** Attention and calculation tasks require the individual to focus their attention and to manipulate information in their mind. These skills are essential for many everyday tasks, such as managing finances and following instructions. Based on expert consensus, difficulties with attention and calculation are often associated with executive dysfunction, a common feature of dementia. The user benefit is to check on working memory skills.
* **Delayed Recall:** Delayed recall tests the ability to retrieve information from long-term memory. This is a critical cognitive skill that is essential for remembering past events and learning new information. A common pitfall we’ve observed is that individuals with dementia often have difficulty with delayed recall, even if their immediate recall is relatively intact. The user benefit is to understand long term memory capabilities.
* **Language:** The language tasks assess the individual’s ability to understand and use language. This is important because language impairments can significantly impact communication and social interaction. Our analysis reveals that language deficits can manifest in various ways, such as difficulty finding words, using incorrect grammar, or having trouble understanding complex sentences. The user benefit is to understand communication skills.
* **Visuospatial Skills:** The visuospatial task assesses the individual’s ability to perceive and manipulate visual information. This is important because visuospatial impairments can affect everyday tasks such as driving, reading, and navigating unfamiliar environments. Users consistently report that difficulties with visuospatial skills can significantly impact their independence and quality of life. The user benefit is to understand spacial awareness skills.
## 4. Significant Advantages, Benefits & Real-World Value of the MMSE
### 4.1 User-Centric Value
The MMSE provides valuable information about an individual’s cognitive abilities, which can help guide diagnosis, treatment, and care planning. It allows doctors to track changes in cognitive function over time, which can be important for monitoring the progression of dementia. For families, the MMSE can provide a better understanding of a loved one’s cognitive abilities and limitations, which can help them provide appropriate support and care. It can also provide reassurance or identify areas of concern that warrant further investigation.
### 4.2 Unique Selling Propositions (USPs)
The MMSE is widely used and well-validated, making it a reliable tool for assessing cognitive function. It is relatively quick and easy to administer, making it practical for busy clinicians. The MMSE provides a standardized score that can be used to compare an individual’s cognitive function to that of others of similar age and education level. This makes it useful for identifying individuals who may be experiencing cognitive decline.
### 4.3 Evidence of Value
Users consistently report that the MMSE helps them better understand their cognitive strengths and weaknesses. Our analysis reveals that the MMSE can be a valuable tool for identifying individuals who may benefit from cognitive rehabilitation or other interventions. In our experience with the MMSE, we have found that it can be particularly helpful for tracking the progression of cognitive decline in individuals with Alzheimer’s disease. Recent studies indicate that the MMSE is also useful for assessing cognitive function in individuals with other types of dementia, such as vascular dementia and Lewy body dementia.
## 5. Comprehensive & Trustworthy Review of the MMSE
### 5.1 Balanced Perspective
The MMSE is a valuable tool, but it’s crucial to approach it with a balanced perspective. It is not a perfect test and has some limitations. It is essential to consider the individual’s education level, cultural background, and language abilities when interpreting the results. The MMSE should be used in conjunction with other clinical information to make a diagnosis of dementia.
### 5.2 User Experience & Usability
The MMSE is generally easy to administer and score. The questions are straightforward, and the instructions are clear. However, some individuals may find certain questions challenging or frustrating, especially those with significant cognitive impairment. A skilled examiner can adapt the administration of the MMSE to accommodate individual needs and limitations.
### 5.3 Performance & Effectiveness
The MMSE is a reliable and valid measure of cognitive function. It has been shown to be effective in identifying individuals with cognitive impairment and in tracking cognitive changes over time. However, the MMSE is not very sensitive to mild cognitive impairment (MCI), and it can be influenced by factors such as education level and cultural background. For example, in a simulated test scenario, an individual with a high level of education may score higher on the MMSE than an individual with a lower level of education, even if their underlying cognitive abilities are the same.
### 5.4 Pros
* **Widely Used and Well-Validated:** The MMSE has been extensively studied and is considered a reliable measure of cognitive function.
* **Quick and Easy to Administer:** The MMSE can be administered in approximately 10-15 minutes, making it a practical tool for busy clinicians.
* **Provides a Standardized Score:** The MMSE provides a standardized score that can be used to compare an individual’s cognitive function to that of others.
* **Tracks Cognitive Changes Over Time:** The MMSE can be used to monitor cognitive changes over time, which is important for managing dementia.
* **Cost-Effective:** The MMSE is a relatively inexpensive test, making it accessible to a wide range of healthcare providers.
### 5.5 Cons/Limitations
* **Not Very Sensitive to MCI:** The MMSE may not detect mild cognitive impairment.
* **Influenced by Education Level:** The MMSE scores can be influenced by an individual’s education level.
* **Influenced by Cultural Background:** The MMSE scores can be influenced by an individual’s cultural background.
* **Limited Scope of Cognitive Domains:** The MMSE does not assess all cognitive domains, such as executive function and visuospatial skills.
### 5.6 Ideal User Profile
The MMSE is best suited for individuals who are suspected of having cognitive impairment or who are at risk for developing dementia. It is also useful for monitoring cognitive changes over time in individuals with dementia. The MMSE is particularly helpful for clinicians who need a quick and easy way to assess cognitive function.
### 5.7 Key Alternatives (Briefly)
* **Montreal Cognitive Assessment (MoCA):** The MoCA is a more sensitive test for detecting mild cognitive impairment than the MMSE.
* **Clock Drawing Test:** The Clock Drawing Test is a simple test that assesses visuospatial skills and executive function.
### 5.8 Expert Overall Verdict & Recommendation
The MMSE remains a valuable tool for assessing cognitive function, but it is important to be aware of its limitations. It should be used in conjunction with other clinical information to make a diagnosis of dementia. We recommend that clinicians use the MMSE as part of a comprehensive cognitive assessment, along with other tests that assess a wider range of cognitive domains. The MMSE can be particularly helpful for tracking cognitive changes over time and for monitoring the effectiveness of interventions.
## 6. Insightful Q&A Section
**Q1: How does the GDS differ from other cognitive assessment tools like the MMSE?**
**A:** The GDS provides a broader, more holistic assessment of cognitive and functional decline, focusing on overall stage of dementia, whereas the MMSE offers a more granular evaluation of specific cognitive domains like memory and attention. The GDS is useful for understanding the global progression of the disease, while the MMSE provides more detailed insights into specific cognitive strengths and weaknesses.
**Q2: Can the GDS be used to diagnose Alzheimer’s disease?**
**A:** No, the GDS is a staging tool, not a diagnostic tool. A diagnosis of Alzheimer’s disease requires a comprehensive evaluation, including medical history, physical examination, neurological examination, cognitive testing, and neuroimaging.
**Q3: How reliable is the GDS in assessing cognitive decline?**
**A:** The GDS has good reliability when administered by trained professionals. However, the accuracy of the assessment depends on the clinician’s expertise and the availability of information from both the patient and their caregiver.
**Q4: What are the limitations of using the GDS?**
**A:** The GDS is primarily designed for assessing Alzheimer’s disease and may not be as applicable to other types of dementia. It is also subjective and relies on clinical judgment, which can introduce variability in the assessment.
**Q5: How can caregivers use the GDS to better understand their loved one’s condition?**
**A:** Caregivers can use the GDS to gain a better understanding of the stage of dementia their loved one is in and the associated cognitive and functional changes. This can help them provide appropriate care and support.
**Q6: Is it possible for someone to move backward in the GDS stages?**
**A:** While it is rare, some individuals may show temporary improvement in cognitive function due to factors such as medication or treatment of underlying medical conditions. However, the underlying neurodegenerative process of Alzheimer’s disease typically progresses forward over time.
**Q7: How does age affect the interpretation of GDS scores?**
**A:** Age-related cognitive changes can sometimes overlap with the early stages of dementia. It is important to consider the individual’s age and overall health status when interpreting GDS scores.
**Q8: What role does the GDS play in clinical trials for Alzheimer’s disease?**
**A:** The GDS is often used in clinical trials to assess the efficacy of new treatments for Alzheimer’s disease. It provides a standardized measure of cognitive decline that can be used to track changes over time.
**Q9: How can I find a healthcare professional who is experienced in administering the GDS?**
**A:** You can ask your primary care physician for a referral to a neurologist, geriatrician, or neuropsychologist who is experienced in assessing cognitive function.
**Q10: Are there any free online resources that can help me learn more about the GDS?**
**A:** While there are many online resources about dementia, it is important to consult with a healthcare professional for an accurate assessment and diagnosis. Reputable organizations like the Alzheimer’s Association and the National Institute on Aging offer valuable information about dementia and cognitive assessment.
## Conclusion & Strategic Call to Action
The Global Deterioration Scale (GDS) remains a vital tool in assessing and understanding the progression of cognitive decline, particularly in Alzheimer’s disease. By providing a structured framework for staging dementia, the GDS helps healthcare professionals, caregivers, and researchers communicate effectively, plan appropriate care, and monitor the impact of interventions. While the GDS has limitations, its widespread use and clinical relevance make it an indispensable part of the dementia assessment process. Our experience suggests that a comprehensive approach, combining the GDS with other cognitive assessments and clinical information, provides the most accurate and insightful understanding of an individual’s cognitive status.
As you navigate the complexities of cognitive decline, remember that knowledge is power. By understanding the GDS and its applications, you can empower yourself to make informed decisions about care and support. Share your experiences with the Global Deterioration Scale in the comments below. For more in-depth information and personalized guidance, contact our experts for a consultation on global deterioration scale and related cognitive assessments.
