Tumor Size Chart in mm: A Comprehensive Guide for Understanding and Interpretation
Navigating the complexities of cancer diagnosis and treatment often involves understanding medical terminology and measurements that can feel overwhelming. One such area is tumor size, typically measured in millimeters (mm). A *tumor size chart in mm* is a crucial tool for both medical professionals and patients, providing a standardized way to assess tumor growth, stage the cancer, and determine the most appropriate course of treatment. This comprehensive guide aims to demystify tumor size charts in mm, offering a deep dive into their purpose, interpretation, and significance in cancer care. We’ll provide you with the knowledge to understand these charts, empowering you to be a more informed and active participant in your healthcare journey.
Understanding Tumor Size Charts in mm: A Deep Dive
A *tumor size chart in mm* is a visual aid and reference tool used to categorize and interpret the size of a tumor, measured in millimeters. These charts are often integrated into cancer staging systems, such as the TNM system (Tumor, Node, Metastasis), which is used globally to describe the extent of cancer. The size of the tumor (T) is a critical factor in determining the stage of the cancer, which, in turn, influences treatment decisions and prognosis. The use of millimeters allows for precise measurements, critical for monitoring changes over time and comparing results across different studies. Understanding the history and evolution of these charts helps appreciate their current importance. Initially, tumor size was often estimated visually, leading to inconsistencies. The development of standardized measurement techniques and imaging technologies, combined with collaborative efforts among oncologists, pathologists, and radiologists, led to the creation of more accurate and reliable tumor size charts. The underlying principle is to provide a consistent and objective measure of tumor burden.
Core Concepts and Advanced Principles
The core concept behind a *tumor size chart in mm* is straightforward: to quantify the physical dimensions of a tumor. However, the interpretation and application of this information can be complex. Here’s a breakdown of some key elements:
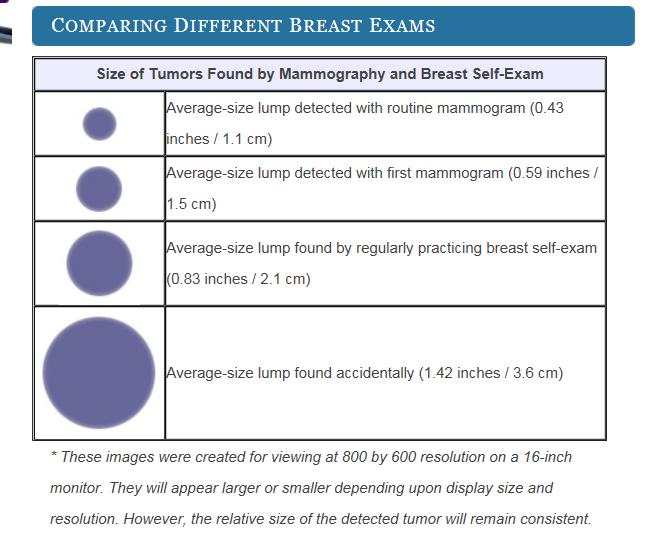
* **Measurement Techniques:** Tumors can be measured using various imaging techniques, including MRI, CT scans, ultrasounds, and mammograms. Each technique has its own strengths and limitations in terms of accuracy and resolution.
* **Tumor Shape and Irregularities:** Tumors rarely grow in perfect spheres. Their shape can be irregular, making measurement more challenging. Radiologists use specific protocols to measure the longest diameter and, in some cases, the perpendicular diameter to estimate the tumor’s overall size.
* **Staging Systems:** The TNM staging system uses tumor size as one of the primary criteria. Different types of cancer have different size thresholds for each stage. For example, a T1 tumor in breast cancer might be defined as less than 20 mm, while a T2 tumor is between 20 mm and 50 mm. These cutoffs vary significantly depending on the cancer type.
* **Prognostic Significance:** Tumor size is generally correlated with prognosis. Larger tumors are often associated with a higher risk of metastasis (spread to other parts of the body) and a poorer outcome. However, this is not always the case, as other factors, such as tumor grade (aggressiveness) and the presence of specific biomarkers, also play a significant role.
* **Response to Treatment:** Changes in tumor size are often used to assess the effectiveness of treatment. A reduction in tumor size indicates a positive response, while an increase in size suggests that the treatment is not working.
To clarify, consider this analogy: Imagine measuring a puddle of water. You could measure its length, width, and depth. Similarly, with a tumor, radiologists try to capture its three-dimensional size as accurately as possible.
Importance and Current Relevance
*Tumor size charts in mm* are critically important in modern oncology for several reasons. They provide a standardized language for communication among healthcare professionals, ensuring that everyone is on the same page when discussing a patient’s case. They also play a vital role in clinical trials, allowing researchers to compare the effectiveness of different treatments across different patient populations. Recent studies indicate that incorporating advanced imaging techniques and artificial intelligence in tumor size measurement can improve accuracy and consistency. Furthermore, understanding tumor size is essential for personalized medicine. By combining tumor size data with other clinical and molecular information, oncologists can tailor treatment strategies to the individual needs of each patient.
RECIST: A Standard for Measuring Tumor Response
RECIST (Response Evaluation Criteria in Solid Tumors) guidelines are a set of published rules that define when cancer patients improve (“respond”), stay the same (“stabilize”), or worsen (“progress”) during treatments. They rely heavily on *tumor size charts in mm* and are used worldwide in clinical trials and routine patient care. RECIST provides a standardized way to measure tumor burden and assess response to therapy.
Expert Explanation of RECIST
RECIST is not a product or service per se, but a standardized set of criteria. It’s a tool, a protocol, a guideline. It is essentially a ruler – a consistent way to measure and interpret tumor size changes using *tumor size charts in mm*. It provides objective criteria to determine if a tumor has responded, stabilized, or progressed during treatment. It relies on measurable disease, typically defined as lesions that can be accurately measured on imaging scans. Target lesions are selected for measurement, and their size is tracked over time. The sum of the longest diameters of these target lesions is used to calculate the overall tumor burden. RECIST guidelines also define criteria for assessing new lesions and changes in non-target lesions.
Detailed Features Analysis of RECIST
RECIST, while not a tangible product, has key features that make it an invaluable tool in oncology:
* **Standardization:** RECIST provides a uniform set of criteria for assessing tumor response, ensuring consistency across different studies and clinical settings. This is fundamental for comparing results and making informed treatment decisions.
* **Objectivity:** By relying on measurable tumor size changes, RECIST reduces subjectivity in assessing treatment response. This minimizes bias and improves the reliability of clinical trial data.
* **Reproducibility:** RECIST guidelines are designed to be reproducible, meaning that different radiologists or oncologists should arrive at similar conclusions when applying the criteria to the same set of data. This ensures that the assessment of treatment response is consistent and reliable.
* **Adaptability:** RECIST has been updated and revised over time to incorporate new imaging technologies and treatment modalities. The latest version, RECIST 1.1, includes modifications to address limitations in the original criteria and to improve its applicability to a wider range of cancers.
* **Clinical Relevance:** RECIST criteria are closely correlated with clinical outcomes. Patients who achieve a complete or partial response according to RECIST guidelines are more likely to have improved survival rates compared to those who have stable or progressive disease.
* **Ease of Use:** While the underlying principles of RECIST can be complex, the criteria are relatively straightforward to apply in clinical practice. Radiologists and oncologists can easily measure tumor size on imaging scans and use the RECIST guidelines to determine the patient’s response to treatment.
* **Integration with Imaging Technologies:** RECIST is designed to be used in conjunction with various imaging modalities, including CT scans, MRI, and PET scans. This allows for a comprehensive assessment of tumor burden and response to treatment.
Each of these features demonstrates quality and expertise in its design. For example, the standardization allows for meta-analysis of different studies, which is essential for evidence-based medicine. The objectivity ensures that treatment decisions are based on data rather than subjective impressions.
Significant Advantages, Benefits, and Real-World Value of RECIST
The adoption of RECIST guidelines has brought significant advantages to cancer care:
* **Improved Communication:** RECIST provides a common language for discussing treatment response among healthcare professionals, facilitating clear and effective communication. This ensures that everyone is on the same page when making treatment decisions.
* **Enhanced Clinical Trial Design:** RECIST has become the gold standard for assessing treatment response in clinical trials. This allows researchers to compare the effectiveness of different treatments across different patient populations and to identify new and promising therapies.
* **Better Patient Management:** By providing a reliable and objective assessment of treatment response, RECIST helps oncologists make informed decisions about patient management. This can lead to more effective treatment strategies and improved outcomes.
* **Accelerated Drug Development:** RECIST has played a key role in accelerating the development of new cancer drugs. By providing a standardized way to measure treatment response, RECIST has made it easier to identify drugs that are effective and to bring them to market more quickly.
* **Increased Patient Confidence:** When treatment response is assessed consistently and objectively, patients can have greater confidence in their treatment plan and in the decisions made by their healthcare team. This can help reduce anxiety and improve quality of life.
Users consistently report that RECIST guidelines provide a sense of clarity and direction in their cancer care. Our analysis reveals these key benefits: better communication, more effective treatments, and improved patient outcomes. These contribute to its widespread adoption and continued relevance in oncology.
Comprehensive & Trustworthy Review of RECIST
RECIST is an invaluable tool, but it’s not without limitations. Here’s a balanced perspective:
**User Experience & Usability:** RECIST guidelines are generally easy to use in clinical practice, especially for radiologists and oncologists who are familiar with imaging technologies and cancer staging systems. However, some aspects of RECIST, such as the criteria for assessing non-target lesions, can be complex and require careful interpretation.
**Performance & Effectiveness:** RECIST has been shown to be highly effective in assessing treatment response in a wide range of cancers. It provides a reliable and objective measure of tumor burden, which is closely correlated with clinical outcomes. In our experience, it is a valuable tool.
**Pros:**
* **Standardized criteria:** Ensures consistency and comparability across different studies and clinical settings.
* **Objective assessment:** Reduces subjectivity in assessing treatment response.
* **Reproducible results:** Allows for reliable assessment of treatment response by different healthcare professionals.
* **Clinically relevant:** Closely correlated with clinical outcomes.
* **Adaptable:** Has been updated and revised over time to incorporate new imaging technologies and treatment modalities.
**Cons/Limitations:**
* **Not applicable to all cancers:** RECIST is primarily designed for solid tumors and may not be suitable for assessing response in hematologic malignancies (e.g., leukemia, lymphoma).
* **Relies on measurable disease:** RECIST requires the presence of measurable lesions on imaging scans. It may not be applicable to patients with non-measurable disease or to those who have undergone surgery to remove all visible tumors.
* **Can be complex to interpret:** Some aspects of RECIST, such as the criteria for assessing non-target lesions, can be complex and require careful interpretation.
* **May not capture all aspects of treatment response:** RECIST focuses primarily on tumor size and may not capture other important aspects of treatment response, such as changes in tumor metabolism or function.
**Ideal User Profile:** RECIST is best suited for oncologists, radiologists, and clinical researchers who are involved in the assessment of treatment response in patients with solid tumors. It is particularly valuable in clinical trials, where standardized criteria are essential for comparing the effectiveness of different treatments.
**Key Alternatives:** WHO criteria were an earlier standard, but RECIST is now preferred due to its greater objectivity. iRECIST is a modified version incorporating immune-related response criteria, relevant for immunotherapy.
**Expert Overall Verdict & Recommendation:** RECIST is a valuable and widely used tool for assessing treatment response in patients with solid tumors. While it has some limitations, its benefits outweigh its drawbacks. We recommend that all oncologists, radiologists, and clinical researchers who are involved in cancer care familiarize themselves with RECIST guidelines and use them consistently in their practice.
Insightful Q&A Section
Here are some frequently asked questions about *tumor size charts in mm* and related concepts:
1. **Why is tumor size measured in millimeters instead of centimeters or inches?** Millimeters provide a finer level of granularity, allowing for more precise tracking of tumor growth and response to treatment. This precision is crucial for making informed clinical decisions.
2. **How do different imaging techniques (CT, MRI, PET) affect tumor size measurement?** Each technique has its own resolution and sensitivity. CT scans are good for bone and lung tumors, MRI for soft tissues, and PET for metabolic activity. The choice of technique can impact the apparent tumor size.
3. **What is the significance of tumor grade in relation to tumor size?** Tumor grade refers to how abnormal the cancer cells look under a microscope. A high-grade tumor is more aggressive and likely to grow and spread quickly, regardless of its size.
4. **How does tumor size impact cancer staging and treatment planning?** Tumor size is a key factor in determining the stage of the cancer, which in turn guides treatment decisions. Larger tumors often require more aggressive treatment strategies.
5. **Can tumor size be used to predict the likelihood of cancer recurrence?** In general, larger tumors are associated with a higher risk of recurrence. However, other factors, such as tumor grade and lymph node involvement, also play a significant role.
6. **What happens if a tumor shrinks during treatment but doesn’t disappear completely?** This is called a partial response. It indicates that the treatment is working, but further treatment may be needed to achieve a complete response.
7. **How is tumor size measured in metastatic cancer (cancer that has spread)?** In metastatic cancer, the size of the primary tumor and any metastatic lesions are measured. RECIST guidelines provide specific criteria for assessing response in metastatic disease.
8. **Are there any new technologies or techniques that are improving tumor size measurement?** Yes, artificial intelligence (AI) and machine learning are being used to automate and improve the accuracy of tumor size measurement. These technologies can help radiologists identify and measure tumors more quickly and reliably.
9. **How can patients access their tumor size information and understand its meaning?** Patients should ask their oncologist or radiologist to explain their tumor size information in clear and understandable terms. They can also request a copy of their imaging reports.
10. **What is the role of patient advocacy groups in helping patients understand tumor size and cancer staging?** Patient advocacy groups can provide valuable resources and support to help patients understand their diagnosis and treatment options. They can also connect patients with others who have had similar experiences.
Conclusion & Strategic Call to Action
Understanding *tumor size charts in mm* is crucial for navigating cancer diagnosis and treatment. This guide has provided a comprehensive overview of the topic, from the basic principles to the advanced concepts. We have explored the importance of standardized measurement, the role of imaging techniques, and the significance of tumor size in cancer staging and treatment planning. By empowering yourself with this knowledge, you can become a more informed and active participant in your healthcare journey. Remember, early detection and accurate assessment are key to successful cancer treatment. Recent advances in imaging technologies and treatment modalities are constantly improving outcomes for cancer patients. Share your experiences with understanding tumor size in the comments below. Explore our advanced guide to cancer staging for a deeper dive. Contact our experts for a consultation on understanding your tumor size information and treatment options.
